Gonadotropin releasing hormone analogs
What are the characteristics of the endogenous Gonadotropin releasing hormone? (GnRH)
GnRH is released from a group of loosely connected neurons of the medical basal hypothalmus.It is released in a pulsatile fashion into the capillary system of the pituitary. Binding specifically to highly sensitive receptors on the anterior pituitary,it causes release of gonadotropins.
Its half life is 2-4 minutes and is degraded by peptidase and cleared by glomerular filtration. To use GnRH clinically, it is important to stabilize the molecule, delay its degradation and hence prolong the duration of action. Hence various changes are made to the chemical composition of the hormone resulting in development of GnRH analogs-both agonist and antagonists.
Gonadotropin releasing hormone agonists (GnRha)
Chemical changes made to the original molecule to make it fit for clinical use include:
- Replacement of Glycine at number 10 at the C-terminus and attachment of NH2-ethylamine to the proline of position 9-Increases the potency.
- Substitution of Glycine by D-amino acids at position 6- Slows down the enzymatic degradation
Mode of action of GnRHa:
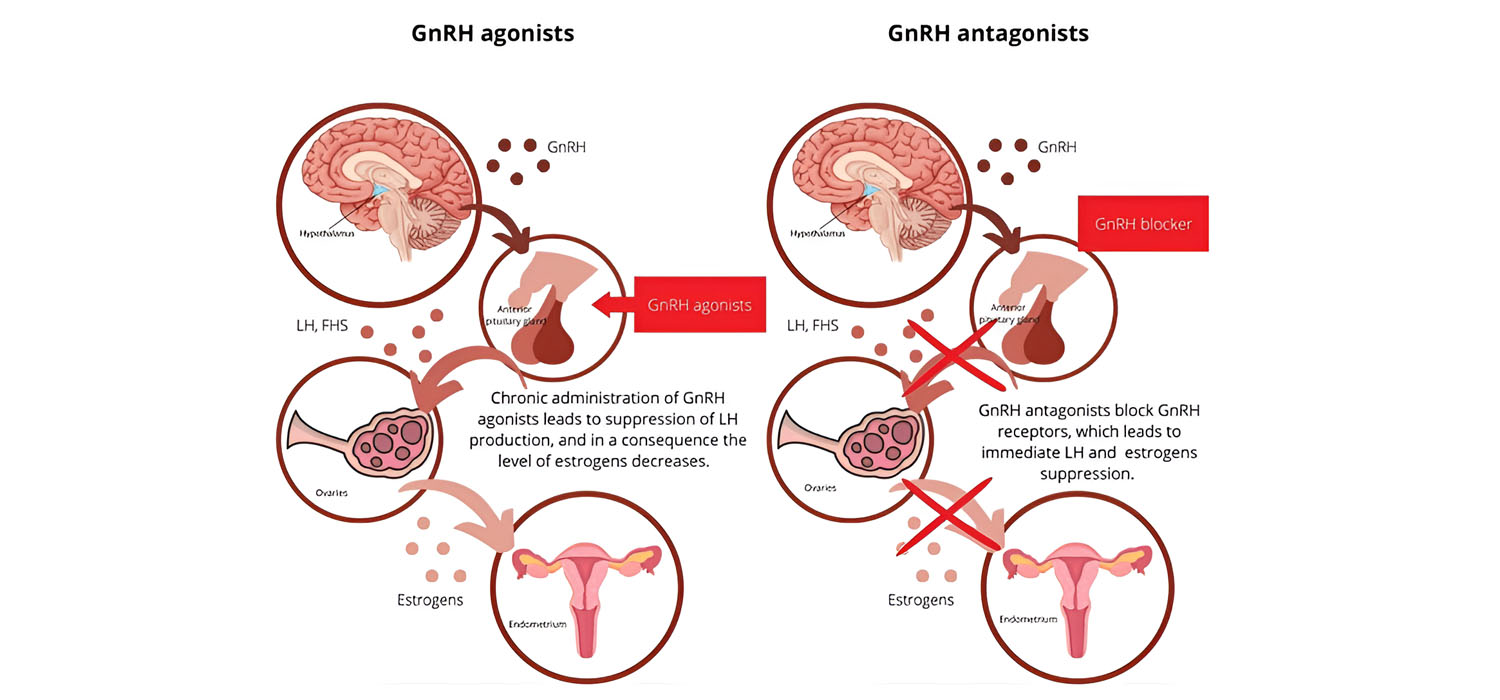
GnRHa bind to the GnRH receptors and cause an initial increase in the secretion of Gonadotropins. This is called the flare effect. However, with sustained administration, the receptor is downregulated as it is internalized via receptor medicated endocytosis. This is sometimes referred to as medical hypophysectomy as there is suppression of both FSH and LH.
Routes of administration of GnRHa:
GnRHa are small polypeptide molecules and cannot be given by oral route. They are administered by subcutaneous, intramuscular and intranasal routes as daily doses. The subcutaneous and intranasal routes are available as depot preparations also.
Gonadotropin releasing hormone antagonists
Substitution of the original amino-acids have been done at multiple positions to the original GnRH for deriving the GnRH antagonist. The substitution in the first three amino acids is what makes them antagonist than agonists.Over 20 years, three generation of antagonists have been developed. The third generations of antagonists ( which have substitution at 8th and 10th position) have significant reduced risk of histamine release and anaphylaxis and hence have been approved for clinical use.
Mode of action of GnRH antagonists:
The GnRH antagonists act by competitive inhibition of the receptors in Pituitary. The action is immediate and inhibition is not prolonged, unlike that of GnRHa. The return to normalcy is also immediate.
GnRH agonist and antagonists -Comparison and Contrasting
| Initial Flare effect | No flare effect |
| Onset of action slow and recovery is also slow | Action sets in within 8 hours. Return to normalcy is also quick |
| Uniform follicular development | Follicular development not uniform |
| Can be used for batch IVF | Cannot be used for batch IVF |
| Can be used as ovulation trigger | No. Cannot be used as trigger |
| Internalizes the receptors and downregulates pituitary response | Competitive inhibition of receptors and pituitary response to gonadotropins preserved |
| Can be used for luteal support | No. Cannot be used for luteal support |
| Symptoms of hypoestrogenism | No |
| Longer duration of stimulation, more gonadotropins needed | Shorter duration of stimulation and less gonadotropins needed |
| Higher risk of OHSS | Lower risk of OHSS |
| Not used in mild or dual protocols | Used in natural, mild, dual protocols |
| Slightly more oocytes obtained | Slightly less oocytes obtained |
Clinical use of Gonadotropin analogs:
The broad categories of use include use in Assisted reproductive technology (ART) and use in other conditions.
Use of GnRH analogs in ART-GnRH agonists
A) GnRHa in Ovulation Induction protocols
GnRHa are used for suppression of the pituitary. This allows for the use of exogenous gonadotropins, prevents premature LH surge and allows the clinician to have cycle control. The various protocols include:
1) Long agonist or the downregulation protocol
GnRHa is started in the mid-luteal phase of previous cycle as a daily dose and is continued through out stimulation in order to achieve suppression of LH surge. This can be used in combination with oral contraceptive pills and is advantageous in preventing functional ovarian cysts and for the programming of IVF cycles.
2) Short agonist protocol
GnRHa is started on day 2 of the menstrual cycle and continued along with the gonadotropins till the ovulation trigger. The initial flare effect that results in the release of gonadotropins also helps the stimulation. However, suppression of LH surge is not as effective as in long protocol. This protocol is associated with decreased oocyte quality and ongoing pregnancy rates compared to the long protocol.
3) Ultrashort and microdose protocols
In the ultrashort protocol GnRHa is administered only for the initial 3 days of stimulation, the gonadotropins being started a day after the GnRHa administration. In microdose protocol, 60-80 mcg of GnRHa is given twice along with gonadotropins and maybe especially useful in poor responders.
B) GnRHa for ovulation trigger
The flare effect caused by GnRHa can be utilized to trigger ovulation. This is especially useful where hCG is contraindicated for the fear of OHSS. (Ovarian Hyperstimulation Syndrome) However use of GnRHa can cause luteal phase insufficiency and this has to be supplemented suitably.
C) GnRHa for luteal phase support
The GnRHa amplifies LH secretion from the anterior pituitary and hence provided luteal support. It also has a direct beneficial action on the endometrial GnRH receptors and the embryo. Modes of use is: Injection Decapeptyl 0.1 mg, sub-cutaneous on Day 5 or 6 of oocyte retrieval or intranasal Nafarelin 200 mg twice daily from the day of oocyte retrieval. Cochrane reviews have suggested an increase in the ongoing pregnancy rates when GnRHa is used along with progesterone than when progesterone is used alone.
Use of GnRH analogs in ART-GnRH antagonists
GnRH antagonists in ovulation induction protocols
GnRH antagonist is added during the process of stimulation with gonadotropins.
In the single high-dose protocol (French Protocol), a single high dose of antagonist (3mg) is administered on day 8 or when the lead follicle is 14mm. This is expected to suppress the LH surge for 3 days.
In the fixed daily dose protocol, GnRHa Cetrorelix 0.25 mg is added daily from the 6th days of cycle till the day of trigger.
The flexible daily dose is when the GnRHa Cetrorelix is administered at a dose of 0.25mg from the day the follicles reaches 14 mm till the day of trigger.
In Modified natural cycle protocols, the antagonist is administered when the follicle is 14mms and before the hCG trigger. No previous medications are given before this. However, FSH/LH can be given after the antagonist. It can be used in poor responders and when there is contraindication for stimulation.
The advantages of including GnRH antagonists in ovulation stimulation are:
- Shorter periods of ovarian stimulation with no preceding long periods of pituitary suppression.
- Physiologic way of ovarian stimulation, integrated in a spontaneous cycle.
- Reduction in the risk of OHSS
Other uses of GnRH analogs
1) Endometriosis - By suppressing the HPO axis, the ovarian steroidogenesis is halted and endometriosis goes into remission. Analogs are used for 4-6 months. Undesirable effects of hypoestrogenism and reduced bone density can be tackled with the use of low dose hormone replacement.
2) Fibroids - Use of LHRH agonists result in 30-40% reduction in size of large fibroids enabling laparoscopic removal. The reduction in size is temporary as there is regrowth within 3 months to the normal size. Also the surgical plane may get altered making removal difficult.
3) Precocious puberty - The GnRH analogs remain the mainstay in the treatment of precocious puberty. Suppression of pituitary gonadal axis ceases sexual development, declines skeletal maturation and decreases the growth rate without undesirable effects.
4) Benign prostatic hyperplasia - In patients at risk for surgery, GnRH agonist reduces the size of prostate to 30% of the original size and improves symptoms of urinary obstruction also. GnRH antagonists also can be used and improvements persist even after stopping its administration probably due to the direct effect of antagonists on the prostatic epithelium and other growth factors.
5) Use in Oncology - Cancers that depend on sex steroid hormones can be treated with GnRH analogs. These include prostate, breast, ovarian and endometrial cancers. Prostate cancer shows the best response to hormone therapy. GnRH analogs can be used alone or in combination with anti-androgens like flutamide.
For more info, Visit : www.medlineacademics.com