Luteal Phase support (LPS)
Luteoplacental shift (Shift from corpus luteal support to placental support) occurs during the 5th week of intrauterine life when placental steroidogenesis begins. However, it continues till the development of a placental system which can entirely sustain the pregnancy. That is by 12-14 weeks.
Why is there a luteal phase defect (LPD) in Assisted reproductive technologies (ART)?
There are various factors that contribute to LPD in ART. They are:
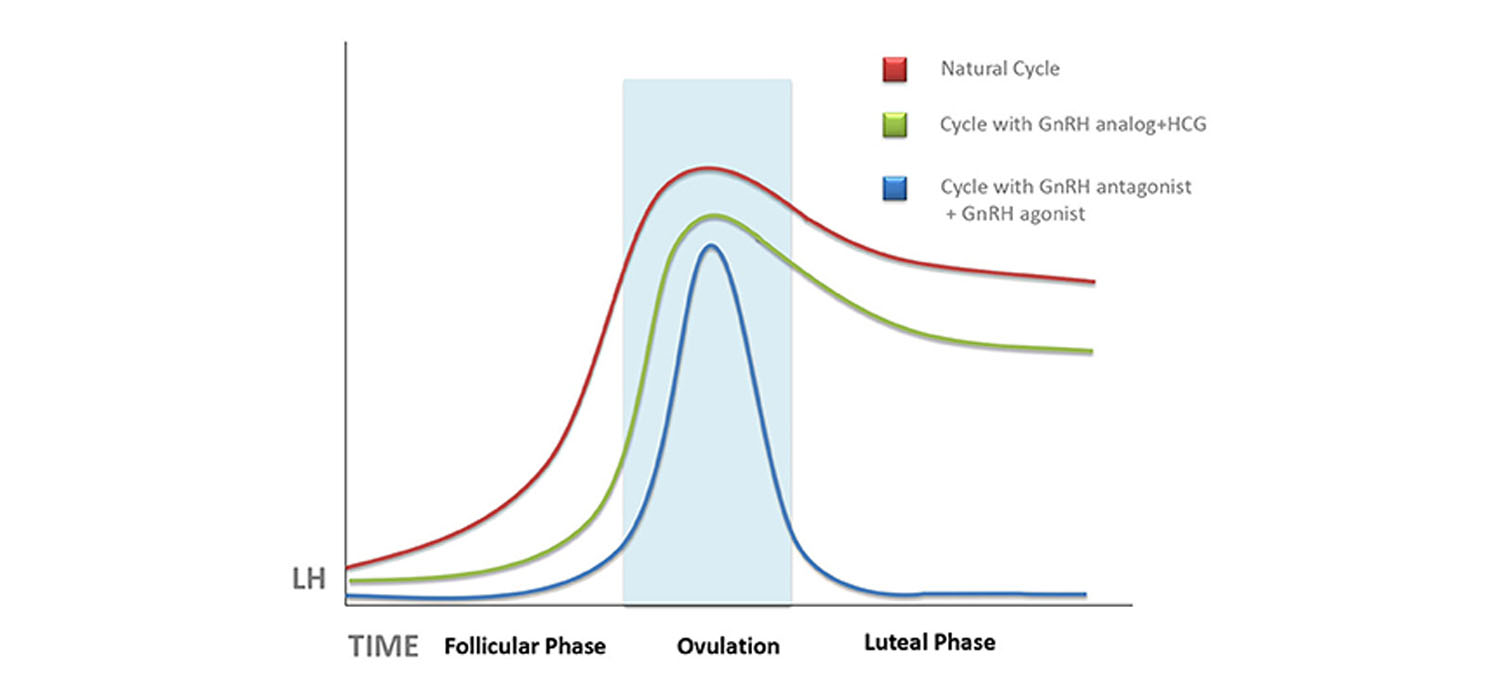
- Supraphysiological levels of ovarian hormones suppress the LH which is important to maintain the corpus luteum
- GnRHa triggers have a short half life and cannot sustain the corpus luteum and can result in premature luteolysis.
- Oocyte retrieval disrupts the cumulus complex with loss of cells that can produce progesterone.
- Downregulation in agonist cycles causes loss of pulsatile LH.
- hCG, when used as a trigger, inhibits endogenous LH secretion.
What is the aim of LPS?
LPS involves the administration of pharmacological agents with the aim of supporting implantation and enhance the chance of pregnancy.
What are the situations in which LPS is indicated?
Luteal phase supportis indicated in:
- Recurrent pregnancy loss ( RPL)
- IVF/ICSI cycles where controlled ovarian stimulation has been used
- Frozen Embryo Transfer (FET) cycles
- IUI cycles where Ovulation Induction has been done with Gonadotropins
- To counter Luteal Phase Defects that can occur in hyperprolactinemia, hypothyroidism, obesity, Auto-immune diseases that affect the hypothalamo pituitary axis, etc.
What are the medications used for LPS?
Progesterone, hCG, GnRHa, Estrogen are some of the medications used for LPS.
1. Progesterone for LPS:
Progesterone induces nitric oxide synthesis in decidua to increase local vasodilatation and causes muscular quiescence. It is used as micronized progesterone or as synthetic progesterone.
Micronized progesterone:
This can be administered by oral, vaginal, rectal and parenteral routes.
Oral micronized progesterone has reduced bio-availability (<10%) due to first pass through liver. Higher doses needed to overcome this cause headache, hypotension, vertigo and sedation. Hence not popular.
Vaginal preparations are available as tablets, suppositories, 8% gel and spray. These avoid first pass and have a local action and also reach greater endometrial concentrations.
The Intramuscular progesterone injections are painful, can irritate skin and cause inflammation and abscess formation. The sub-cutaneous preparations are aqueous and avoid pain.
Transdermal progesterone formulations are not possible as the 5 alpha reductase present in skin deactivates the progesterone.
Synthetic progesterone- Dydrogesterone
Dydrogesterone is highly progesterone receptor selective, lacks androgenic, estrogenic and corticosteroid properties and can be administered orally. It has been found to be non-inferior to micronized progesterone.
2. hCG for LPS
hCG has a longer half-life, can be administered as intramuscular or subcutaneous and is available as urinary and recombinant hCG. There has been no difference in pregnancy and live birth rates between progesterone and hCG. However, hCG is associated with OHSS and must be used with caution.
3. GnRH agonists (GnRHa) for LPS
GnRHa increase LH secretion, have a direct effect on endometrial GnRH receptors and on the embryo. They can be administered as subcutaneous, intramuscular and intranasal preparations. Increased live birth rates have been noted by using GnRHa with progesterone than with progesterone alone.
What is the optimal timing of LPS?
Luteal support if given early, causes advancement of endometrial maturation. Hence it is acceptable to start luteal support 24-48 hours after oocyte retrieval. It is also to be noted that prolongation of luteal support beyond the period when beta hCG becomes positive, has no effect on miscarriage/ delivery rates.
LPS in special situations
1) IUI cycles:
LPS is indicated only in those cycles where gonadotropins have been used for ovulation stimulation. There is no benefit of exogenous progesterone in IUI cycles that have used clomiphene citrate for ovulation induction. There is insufficient evidence that progesterone improves outcomes when letrozole has been used for ovulation induction.
2) LPS in IVF cycles
Fresh transfer cycles where GnRHa trigger has been used, LPS may be modified as:
a) Giving hCG in a dose of 1500 IU after GnRHa trigger. Pregnancy rates are comparable to using on hCG trigger with an associated reduction in OHSS. Another bolus dose of 1500 IU of hCG is given after four days. It is not necessary to give additional progesterone.
b) rLH-300IU is given on alternate days from the day of oocyte retrieval along with vaginal progesterone. It is costly and needs more studies.
c) Intensive progesterone and estrogen support-need more studies
3) LPS in FET cycles
Vaginal progesterone improves pregnancy rates in FET cycles and is started form the day of oocyte retrieval.
Adjuvants in LPS
| Medication | Rationale for use | Evidence | |
|---|---|---|---|
| 1 | IvIg | Inhibiting NK cells, Correcting Th1/Th2 ratio | Doesn’t support use |
| 2 | Anti-TNF Alpha | Increases TNF alpha: Interleukin ratio | Doesn’t support use |
| 3 | IV lipids | Reduce cytotoxic effect of NK cells. Inhibit TH1 cytokines | Routine use not recommended |
| 4 | Steroids | Anti-inflammatory | Limited evidence in auto-immune disorders/ Unexplained RIF & conventional IVF |
| 5 | Low dose Aspirin | Immunosuppressive, increases uterine blood flow and endometrial receptivity | Limited evidence for use in RPL No evidence for routine use |
| 6 | LMWH | Anti-thrombotic effect | Useful in women with thrombophilia Not for routine use |
| 7 | Metformin | Modulates Insulin Like Growth Factor | For women with PCOS undergoing IVF, to reduce risk of OHSS |
| 8 | Myo-Inositol | Acts on Insulin, FSH and LH receptors | Important role in development of oocytes and embryos |
| 9 | Probiotics | Reduce IL-6 and C-Reactive proteins. Increase IL-10 | For women with PCOS undergoing IVF |
| 10 | L-Arginine | Activates immune system. Increases uterine blood flow | Given in patients with thin endometrium |
In conclusion:
Luteal phase support is an important aspect of Assisted Reproductive Techniques. It is especially indicated in those cycles where gonadotropins have been used and in IVF/ICSI cycles. The LPS can be individualised considering the induction protocols, risks of OHSS etc. Several adjuvants when used judiciously and individualised also help in bettering the outcomes.
For more info, Visit : www.medlineacademics.com