Assessment of ovarian reserve
What is ovarian reserve? Why is it important?
Ovarian reserve is the quantity & quality of the primordial follicle pool and is an important factor in determining the fertility of a woman.
Estimation of ovarian reserve assists in making informed decisions about fertility, need for active management and fast-tracking towards IVF.
What is Ovarian Reserve Test (ORT)?
ORT is used to assess the ovarian reserve in a woman. An ideal ORT should be cheap. Easy to perform, reproducible, non-invasive and must accurately measure the reserve pool and should be able to predict the chances of pregnancy.
What are the various ORTs?
ORTs can be broadly classified as bio-chemical, bio-physical, and histological.
Biochemical ORTs
The static biochemical ORTs include menstrual day 2-4 FSH, baseline estradiol, serum inhibin and AMH (Anti-Mullerian Hormone)
The dynamic bio-chemical tests include CCCT (Clomiphene citrate challenge test), EFFORT (Exogenous follicle stimulating hormone ovarian reserve test) and GAST (Gonadotropin- releasing hormone agonist stimulation test). These tests are expensive and time consuming.
Bio-physical ORTs:
Using Ultrasound to assess ovarian reserve constitutes bio-physical ORT, The AFC 9 antral follicular count), ovarian volume and doppler constitute the various aspects of ultrasonographic assessment of ovarian reserve.
Histology:
Ovarian biopsy and histologic examination.
How are the ORTS interpreted?
1) Biological age of the woman:
Age of the woman is the most important predictor of her reproductive potential. It is well known hat fecundity reduces with increasing age of the woman.
2) Baseline FSH.
The specimen is drawn during 2nd to 4th day of menstrual cycle in the morning hours. 10-12 IU/L is regarded as the cut-off, though there doesn’t exist a universal consensus on this. FSH levels exhibit diurnal, intra and inter-cycle variations in the same individual. This cannot be taken as the sole test for ORT because fertility begins to decline several years before the fall of FSH levels and the significance of raised FSH in young, infertile woman with regular cycles is not understood.
3) Serum Estrogen (E2)
E2 when measured along with FSH reflects the ovarian reserve more precisely because increased E2 can mask abnormal FSH levels. Basal E2 levels over 80 pg/ml predicts poor ovarian response. As it does not add to the predictive value of other ORTs, estrogen estimation is not done routinely.
4) Serum Inhibin-B
Inhibin is a glycoprotein produced by the granulosa cells of the follicles. Values below 45pg/ml predict poor response. The unreliability of assays and availability of better predictors like AMH (Anti- Mullerian Hormone) limits the use of Inhibin estimation.
5) AMH
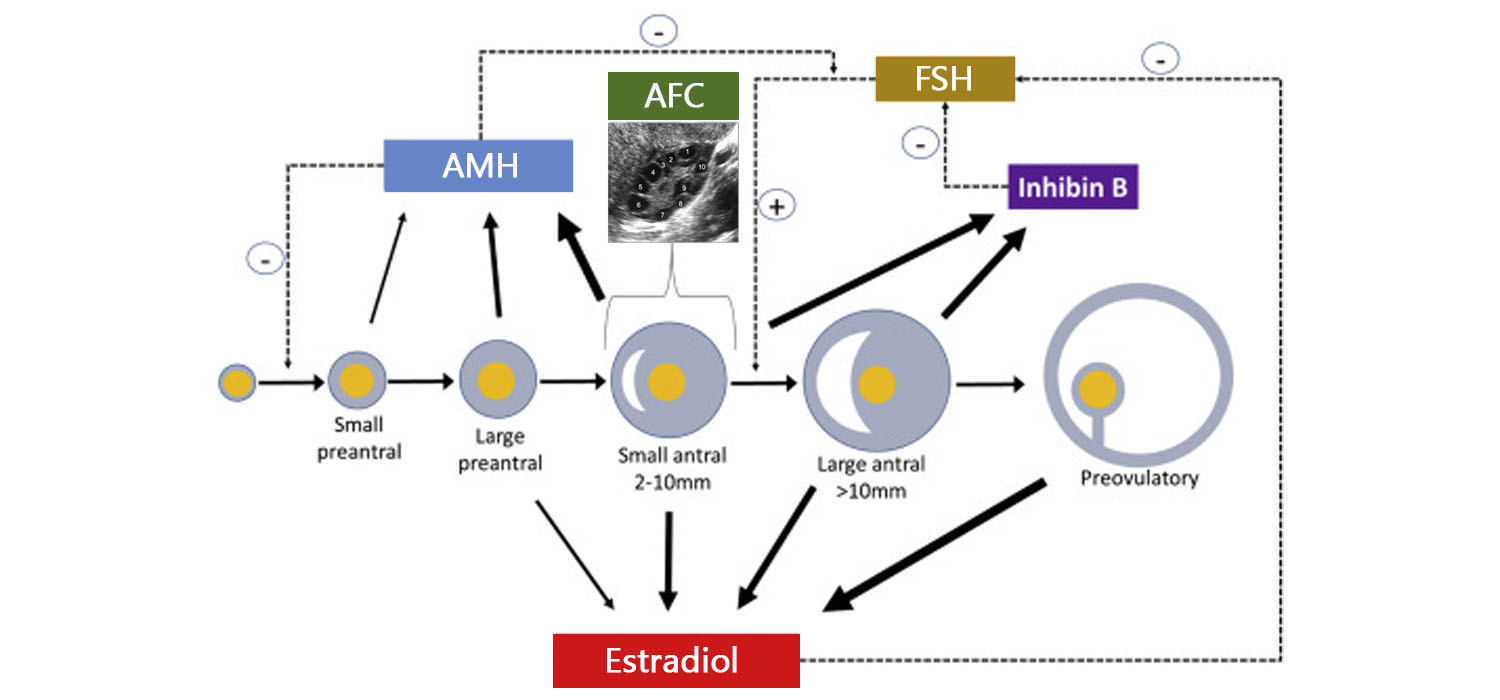
AMH is a dimeric glycoprotein secreted from the granulosa cells of pre-antral follicles and small antral follicles (2-6 mms). It is a regulator of follicular recruitment. Hence falling AMH levels accelerates recruitment of follicles from the primordial group.
AMH can be measured any time of the cycle and there is little intra- or inter- cycle variations. Fully automated assays are available, which take less time and allow international comparison. AMH strongly correlates with the antral follicle count (AFC) and is also the earliest marker to show decline in ovarian reserve. It is a sensitive marker to predict hyper response and can be applied as a screening test in sub-fertile women. It is the only marker which is reliable in assessing fertility after gonadotoxic therapy in young cancer survivors. Age related nomograms are available and can be used to counsel patients. Women with low AMH are advised to prioritize conception or oocyte cryopreservation.
6) CCCT
Basal FSH is done on Day 2 of menstrual cycle following which clomiphene Citrate is given at the dose of 100 mgs/ day for 5 days. FSH is repeated on the 10th day. Increased FSH on day 10 or increased sum of FSH on day 3 and day 10 is evidence of poor ovarian reserve.
Practice points
7) EFFORT
FSH and E2 are estimated on 3rd day of menstrual cycle after which 300IU of FSH is given and E2 tested after 2 hours. Though it can predict hyper-response, it has high false positive rates.
8) GAST
E2 is estimated on day 2 of menstrual cycle followed by administration of 100 microgram of Triptorelin. E2 tested again after 24 hours. Increased value indicates good ovarian reserve.
9) Ultrasound markers of ORT
a) AFC (Antral follicle count)
2-10 mm follicles in the ovary constitute the antral follicles. AFC is measured on the second day of the menstrual cycles using a transvaginal probe of 7.5m Hz. Two perpendicular measurement of each follicle is taken, and the mean is considered as the diameter of the follicle. During IVF cycles, AFC (from both ovaries) less than 8 indicates poor response, 8-16 predicts normal response and over 16 follicles is highly predictive of hyper-response. AFC correlates strongly with AMH and correlates well with age, ovarian reserve, and response to stimulation. There is no advantage of using 3D over 2D for evaluating the AFC.
b) Ovarian volume
Measuring ovarian volume does nota dd value to predicting ovarian reserve
c) Doppler of the Ovaries
The role of ovarian doppler as an ORT method is limited. It can be used to assess the peri-follicular flow during stimulation.
10) Ovarian biopsy is an invasive method and is no longer used as an ORT.
To conclude.
ORT aids in making decisions about conceiving and oocyte freezing, it helps to individualise controlled ovarian stimulation (iCOS). It helps in aiding fertility estimation and potential in women who are cancer survivors. Finally, by aiding early identification of poor ovarian response; clinicians can resort to IVF faster and reduce the time to pregnancy.
For more info, Visit : www.medlineacademics.com