Ovulation triggers
Ovulation triggers are preparations that trigger a cascade of events that result in maturation and release of developmentally competent oocyte from a pre-ovulatory Graafian follicle. In a natural cycle the ovulation trigger is the mid-cycle trigger of LH and FSH occurring from the pituitary.
Physiology of Ovulation
In a natural cycle, the gradual increase in follicle size is brought about by the FSH. The increased estrogen hormone, by negative feedback on the hypothalamo-pituitary axis, causes suppression of further increase in FSH and also signals for the LH increase.
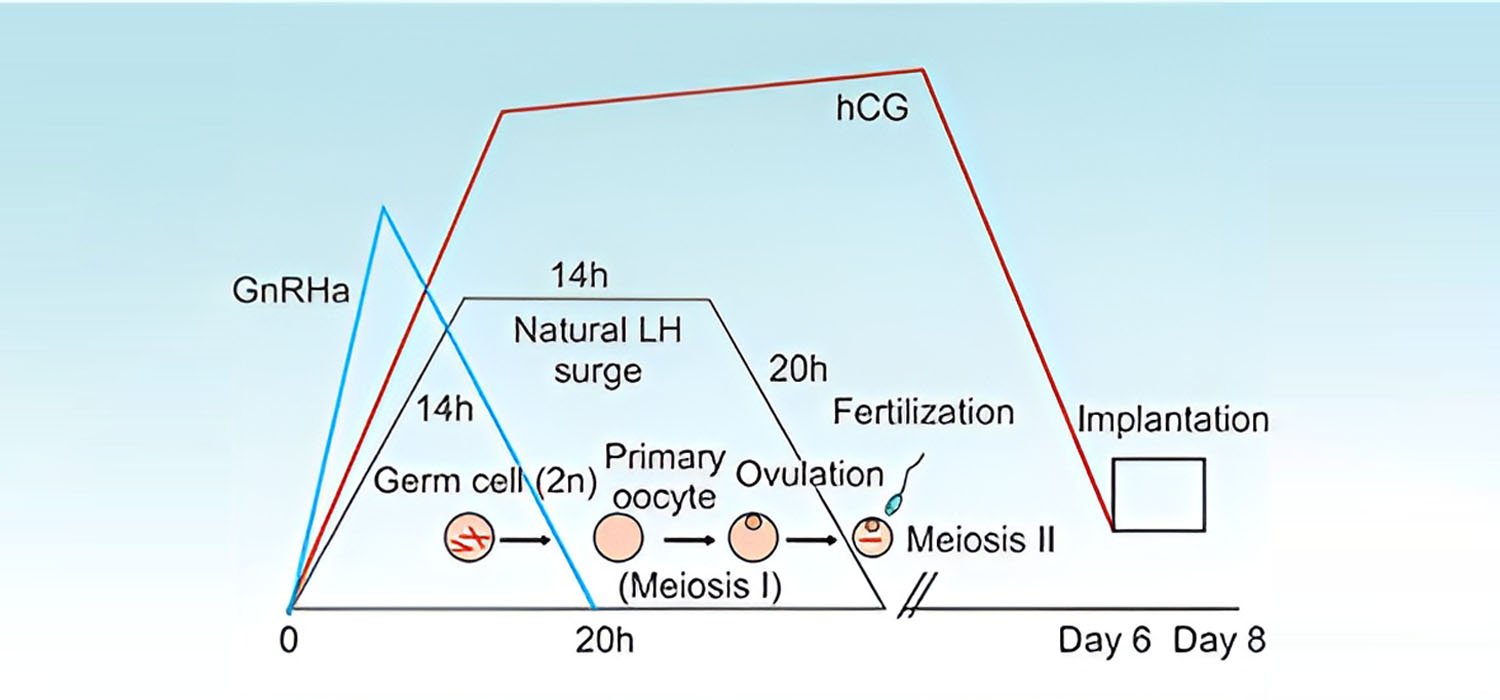
The mid-cycle LH surge is responsible for ovulation. The LH surge lasts for about 48-50 hours and follows the three phases. The ascending phase of 14 hours, the plateau phase of 14 hours when the peak levels are sustained, and the descending phase over the next 20 hours reaches the original value. Hence, ovulation occurs 28-36 hours after the LH starts to rise or around 10-12 hours after the LH peaks.
The mid-cycle LH surge is also accompanied by a small FSH surge, the significance of which is unclear. Thus, the gonadotropin surge initiates a cascade that culminates in ovulation.
Functions of LH at ovulation
- Breakdown of germinal vesicle
- Resumption of meiosis in oocyte- Oocyte progresses from diplotene stage of prophase one and arrests again at metaphase of second meiotic division till fertilization.
- Expansion of cumulus and loss of gap junctions between cumulus cells and oocyte.
- Luteinization of granulosa cells and secretion of progesterone
- Secretion of eicosanoids and prostaglandins necessary for follicular rupture.
- The increased progesterone secretion causes distension of the follicle wall and a pre-ovulatory FSH surge.
Ovulation triggers in IUI and IVF
Since ovulation occurs 36 hours after trigger, it helps to time the IUI.
Oocyte retrieval is undertaken 34-36 hours after the ovulation trigger.
Pharmacological options for Ovulation trigger.
- Urinary hCG (uhCG)
- Recombinant hCG (rhCG)
- GnRH agonist
- Recombinant LH (rLH)
- Dual triggers (hCG + GnRH agonist)
- Kisspeptins
Details of various triggers
| Trigger | Dose and timing | Advantages | Disadvantages | Comments |
|---|---|---|---|---|
| hCG |
|
|
Risk of OHSS | ESHRE recommends urinary or recombinant hCG as equally effective |
| r-LH | 15-30K IU |
|
|
ESHRE does not recommend r-LH for use as trigger |
| GnRHa | Triptorelin-0.2 mg or Lupride 1-1.5mg Or Buserelin 0.5 mg |
|
|
ESHRE (2019) recommends Triptorelin 0.1-0.4mgs |
| Dual trigger | hCG 1-2.5K and GnRHa |
|
|
|
| Kisspeptin |
|
Predictors of success after GnRHa triggers.
Serum E2 > 4000pg/ml, increased LH levels on the day of trigger, number of follicles on the day of trigger determine the success of the trigger.
Trigger preferences in special conditions:
- In oocyte donors-GnRHa
- In Ca Breast patients- GnRHa with use of aromatase inhibitors with gonadotropins for ovulation induction
- Patients with risk of OHSS, Oocyte donors, when PGD is contemplated and in Frozen Embryo transfer cycles-GnRHa
However, no difference has been noted between hCG and GnRHa in terms of oocyte and embryo quality. The greatest advantage of not using hCG trigger is avoiding OHSS.
For more info, Visit : www.medlineacademics.com