Empty Follicle Syndrome (EFS)
EFS is a condition that is encountered at the time of oocyte retrieval wherein despite repeated flushing and aspiration no oocytes are obtained in a cycle that has been adequately stimulated.
The incidence of EFS has been variously quoted as 0.045 to 7%. There is a 20% chance of recurrence in future cycles.
EFS can be categorized as False EFS (FEFS) or Genuine EFS (GEFS)
Who are the patients at high risk of EFS?
Increased age of the woman, obesity, longer duration of infertility, ovaries resistant to various stimulations, greater baseline FSH, reduced estrogen levels on the day of trigger, previous EFS, are some of the risk factors for EFS.
What causes EFS?
FEFS is a classic example of inappropriate formulation and usage of ovulation triggers- “Pharmaceutical Industry Syndrome”! It is more common than GEFS.
FEFS when using hCG trigger can be because of a sub-standard formulation/ improper storage of hCG, improper timing of trigger, patient failing to take the trigger, improper reconstitution of the drug, inappropriate absorption of the drug and improper timing of oocyte retrieval (less than 34 hours or more than 38 hours) Sub-clinical hypogonadotropic conditions may explain FEFS in patients taking GnRHa triggers.
What causes GEFS?
Pathophysiology is poorly understood. Inadequate Hypothalamus secretion, impaired hypothalamo-pituitary axis, and genetic inability to respond to the trigger (LH receptor polymorphism) have been speculated as the reason for GEFS.
Dysfunctional folliculogenesis with predominance of pro-apoptotic factors, ovarian aging, failure of oocyte development and maturation, strong adhesion of oocyte to cumulus complex due to inappropriate paracrine signaling and LH receptor polymorphism causing irreversible bock in LH pathway are some of the proposed mechanisms.
How is the diagnosis of EFS done and how is it managed?
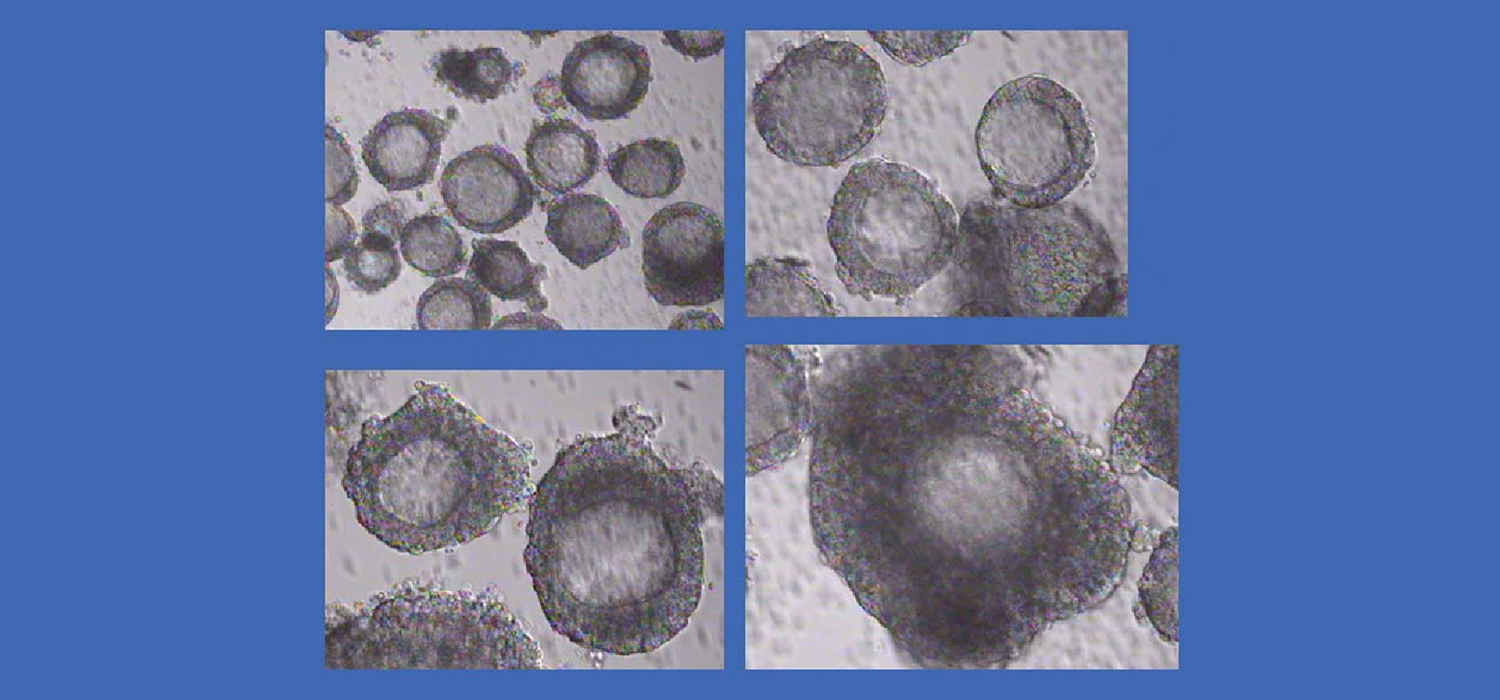
Diagnosis of EFS is at the time of oocyte retrieval when no evidence of oocytes in the aspirated fluid is seen.
When encountering this situation, the aspiration of the other ovary is withheld. In case of hCG trigger, blood, or urine or follicular hCG is measured. If absent or blood hCG is less than 40 mIU/ml, the procedure is abandoned, a second appropriate trigger is given, and oocyte retrieval done after 36 hours. If, however, the hCG levels are found to be appropriate, the other ovary is aspirated. These are cases of GEFS, and they can be offered better stimulation protocols with better triggers or triggers from a different batch in future cycles.
Before subsequent cycles, the patient is re-evaluated for risk factors, recombinant LH or hCG is used for trigger. GnRH Antagonist cycles with GnRHa trigger can be offered.
In case of agonist triggers, a 12-hour post trigger of LH more than 12 mIU/ml is suggestive of appropriate trigger. Reduced progesterone even with normal LH levels means inadequate response.
For more info, Follow : medlineacademics.com