Disorders of puberty - Delayed puberty
The prevalence of delayed puberty is around 3% and it is seen more in boys.
Definition:
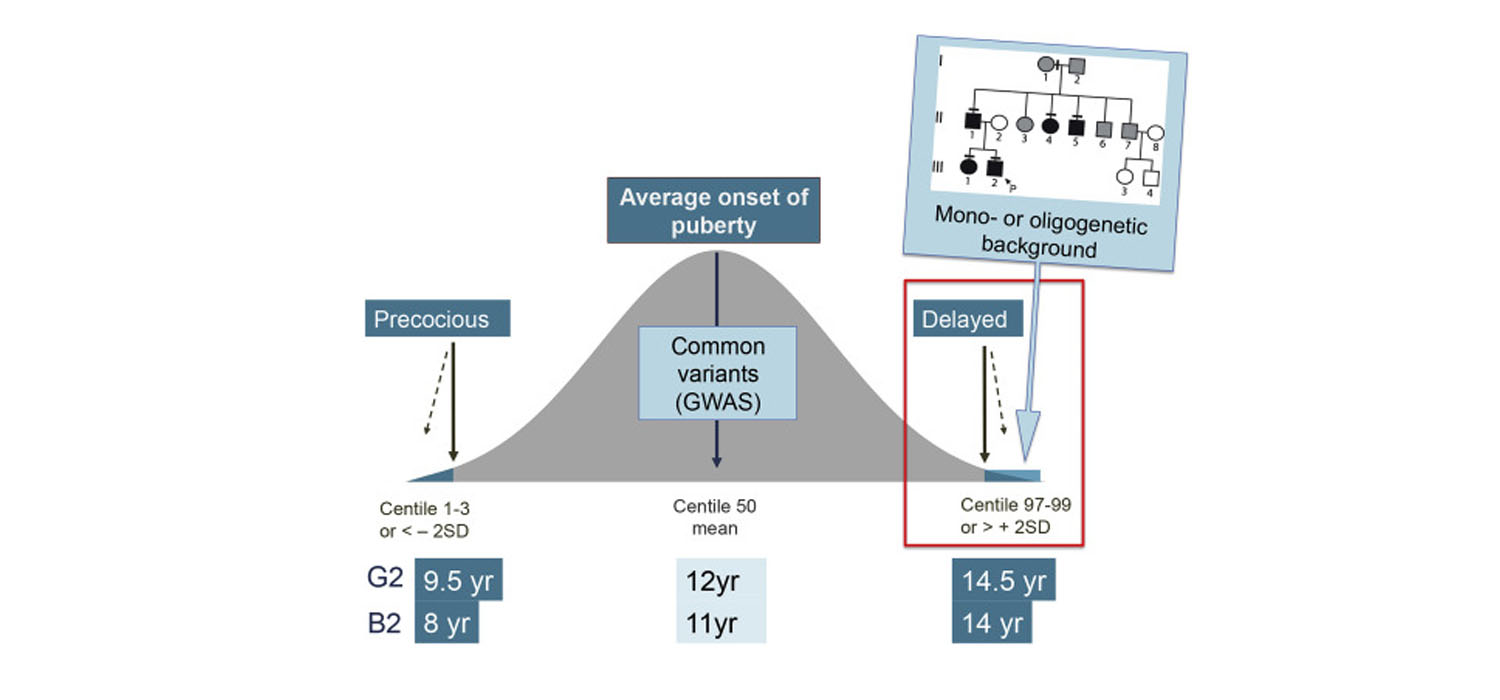
It is the absence of secondary sexual characters by 13 years of age in girls (absent breast development) or by 14 years in boys (no testicular enlargement to at least 4 ml or 2.5cms in length)
Absence of menarche with some pubertal changes by 15 years in girls also demands evaluation. Absence or incomplete development of secondary sexual characters in either sex by 18 years is termed as hypogonadism.
Causes of delayed puberty
1) Constitutional causes
There is often a positive family history of short stature and normal fertility. Chronic diseases, malnutrition, anorexia nervosa, endocrine abnormalities like Type I diabetes mellitus and hypothyroidism can also cause delayed puberty.
2) Hypergonadotropic hypogonadism
Premature ovarian failure/ Oophoritis, Idiopathic testicular failure/ orchitis, anorchia, post chemotherapy, Turner syndrome, Klinefelter’s syndrome.
3) Hypogonadotropic hypogonadism
Hypothalamic or pituitary causes - Inherited-Kallman’s syndromes, Laurence Moon Biedel syndrome
Acquired cause - anorexia nervosa, severe undernutrition, severe exercise, intracranial tumours like craniopharyngioma and prolactinoma, head injury, CNS infection (encephalitis, meningitis) and finally radiotherapy.
4) Normogonadotropic eugonadism
Uterine causes like mullerian agenesis, testicular feminising syndrome, imperforate hymen and PCOS.
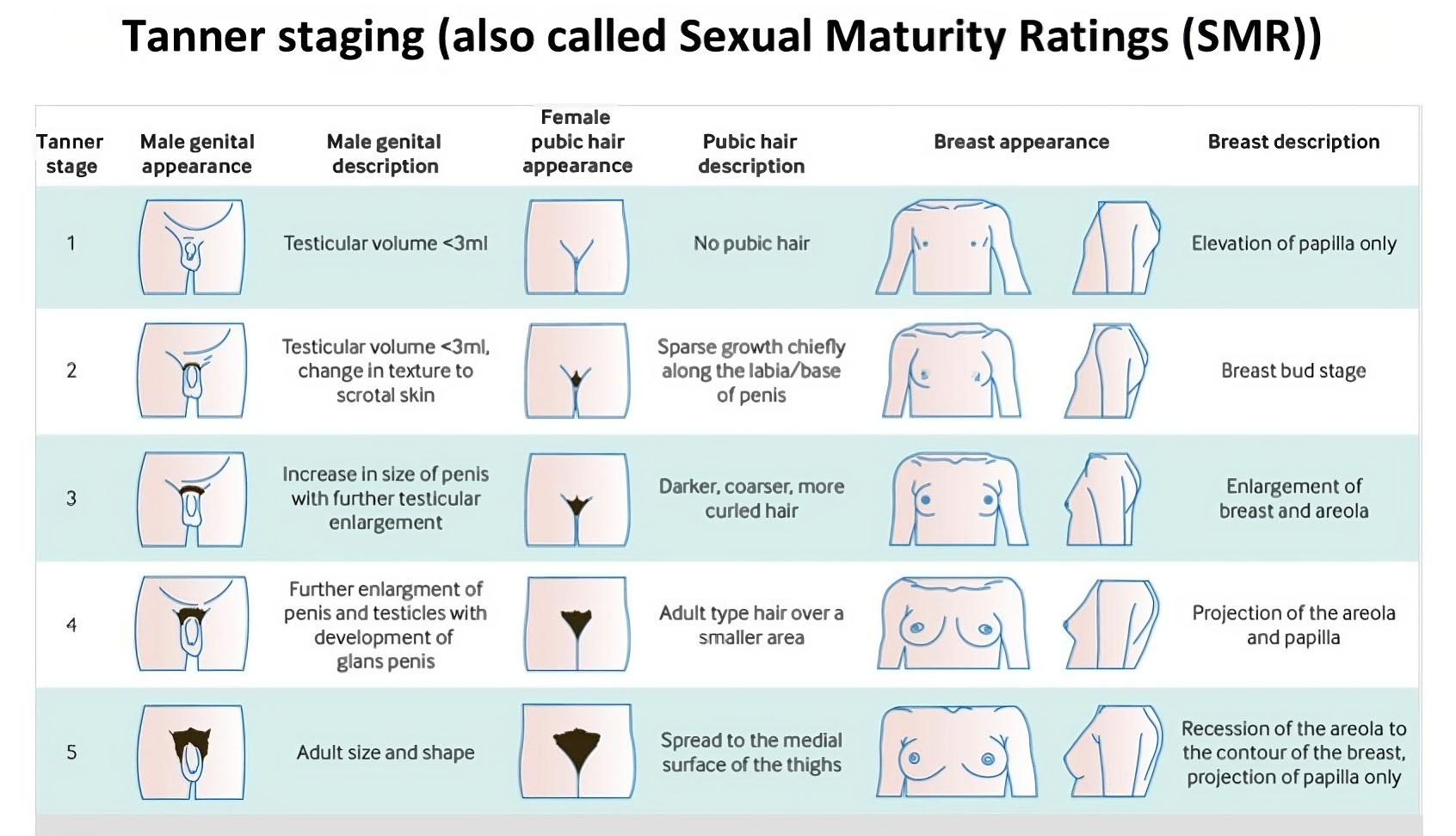
Tanner staging is used to assess the pubertal changes in boys and girls
CDP - Constitutionally delayed puberty - is the most common cause of delayed puberty in over 60% of children when healthy teenagers spontaneously develop puberty after the upper age limit. Delay in puberty can have major psychological impact both on the individual and their parents. Concerns that need to be addressed are any associated pathology, short final adult height, decision about treatment and its duration, and long-term impact on fertility.
Approach to patient with delayed puberty:
Family history of delay in pubertal milestones in older siblings and parents, anosmia can point towards familial cause. Personal history of chronic medical illness like fatigue, pain, abnormal stools suggest underlying metabolic disorders like the inflammatory bowel disease, endocrine or autoimmune disorders.
Physical examination may show the presence of small penis and/or undescended testis which go more in favour of congenital hypogonadotropic hypogonadism. Other features found in syndromic forms of CHH (Congenital Hypogonadotropic hypogonadism) such as Kallmann syndrome are anosmia, cleft lip/cleft palate, and sensory neural deafness, eunuchoid body proportions (arm span exceeding the height by over 5cms) and coloboma of the eyes. In girls, the features of Turner syndrome include short height, web neck, shield chest and cubitus valgus.
Tests such as X-ray of wrist may show that bone age is delayed favouring the diagnosis of CDP.
Basal levels of FSH, LH, Sex steroid is low in CDP and HH while FSH/ LH levels are high in gonadal failure. TSH and prolactin levels also need to be done. GnRH-induced maximal LH levels (cut off is 4.3 mIU/L) is more in CDP than in CHH. Low testicular volume is seen in CHH.
Growth velocity should be charted in all cases. A slow growth velocity of less than 3 centimetres per year goes more in favour of CHH than a functional delay in boys but not so much in girls.
Differentiating between CDP and CHH is challenging. Newer investigations include 36-hour LHRH tests, AMH, Inhibin B.
Pelvic ultrasound may reveal the absence of uterus. MRI is helpful for diagnosing dysgenetic or absent gonads and also for intracranial pathologies.
Karyotyping reveals chromosomal disorders such as Turner syndrome and Klinefelter syndrome. Further genetic analysis may be done when karyotype is normal in order to diagnose rare genetic causes of HH.
Turner syndrome
Genotype - 45 X0 , Incidence is 1:1000 to 2500 girls. It is characterised by hypergonadotropic hypogonadism. Prenatal diagnosis can be done with a combined test in the first trimester and if positive, it is confirmed by amniocentesis or chorionic villus sampling.
Postnatally girls show classic features of short stature, webbed neck, increased carrying angle, cardiac/ renal/ skeletal abnormalities. Treatment is by growth hormone for increasing the height and estrogen and progesterone for inducing puberty. Oocyte donation and IVF can be offered for infertility treatment. As there is association with Coarctation of Aorta, other structural cardiac defects and many systemic disorders, these women are a high risk for obstetrics care. Hence, surrogacy is also indicated in them.
POI (Premature Ovarian Insufficiency) is when there is loss of ovarian activity before 40 years of age. In adolescents, it is often associated with primary amenorrhea. But in some girls with irregular bleeding, the presentation may be misleading as expected menstrual disturbance in adolescents and result in delayed diagnosis of POI.
CHH (Congenital hypogonadotropic hypogonadism) - There exists congenital deficiency of GnRh production in these patients. Abnormal neuronal migration with anosmia is a feature of Kallman syndrome. Kallman syndrome is 4 times more common in males. Anosmia suggests mutation of KAL-1, KAL-2, or KAL-3 genes. CHH can be idiopathic with isolated GnRH secretion deficiency. KISS-1R genetic mutation can also cause CHH.
Treatment
Depends upon the underlying cause.
Correctable causes include supplementation for hypothyroidism, Dopamine agonist for increased prolactin levels, excision of craniopharyngioma and surgical correction of cryptorchidism.
Treatment for Turner syndrome is initiated by 4 years of age. rGH ( recombinant Growth Hormone) therapy is started at a dosage of 0.35- 0.375 milligram/ kg/week by daily subcutaneous injections at night. The patient is monitored with serum IGF-1 levels yearly with aim to keep it at 2 standard deviations above the normal range. The side effects of this therapy include glucose intolerance, intracranial hypertension, stippling of femoral epiphysis and pancreatitis. For girls over 10 years where predicted adult height (PAH) is reduced, rGH with oxandrolone can be given. The side effects include visualization and enlargement of the clitoris and acne. Inducing puberty in these girls can be with Transdermal 17 beta E2 (TDE) given at 3-7 micrograms/day at 11-12 years of age, Cyclic progesterone can be started after 2 years of estrogen therapy or when breakthrough bleeding occurs. These patients need lifelong HRT.
For patients with gonadal failure long term HRT and gamete donation is offered.
For treatment of delayed puberty, HRT is initiated for girls after 13 years and boys after 14 years The goal is induction of virilization or estrogenization, promotion of growth, bone health, libido, and psycho emotional wellbeing. In CDP, further development continues normally after stopping therapy.
In CHH ( Congenital hypogonadotropic hypogonadism) sex steroids are given for induction and maintenance of puberty. This is cheaper than gonadotropin therapy. Gonadotropins may be given for testicular growth and spermatogenesis. hCG is given in the dosage of 1500 to 2000 international units IM biweekly.
Sex hormone replacement is the mainstay for delayed puberty. Oral Testosterone undecanoate should not be used in pubertal induction because of its short half-life. Instead, in males, 500 to 1000 milligrams of testosterone enanthate or cypionate im is used monthly. The patient is monitored every week after injection and the levels are kept in the middle and normal range. For girls overnight transdermal estrogen in the dosage of 6.25 micrograms for 3 to 6 months is given. Dose escalation is individualised. If there are no pubertal changes in 3 to 6 months, the patient must be referred to paediatric endocrinologist.
Extensive counselling is needed for all patients as delayed puberty-constitutional or pathological is challenging to physician and distressing to patients and their parents.
For more information, good practice points and academic excellence, please log onto www.medlineacademics.com and enroll into our FRM (Fellowship in Reproductive Medicine) course.