Uterine factors in infertility - Congenital Uterine abnormalities (CUA)
Uterine factors implicated in infertility affects 1:500 women of reproductive age group. They include uterine polyps, fibroids, adenomyosis, intrauterine adhesions and congenital abnormalities of the uterus.
Prevalence of CUA:
Prevalence in general population is about 4.3-6.7%, in infertile population 3-13% and in patients with recurrent miscarriage, it is 12.6-18.2%.7.7% of women with CUA have chromosomal abnormalities while in 92% it is 46 XX.
Brief embryology of the Uterus
There are three phases of formation and development of uterus. These are organogenesis, fusion and septal resorption. Paramesonephric ducts from either side fuse and grow down and across the mesonephric ducts and develop into the uterus, cervix and upper vaginal. The inter-horn septum is absorbed at around 20 weeks of intrauterine life.
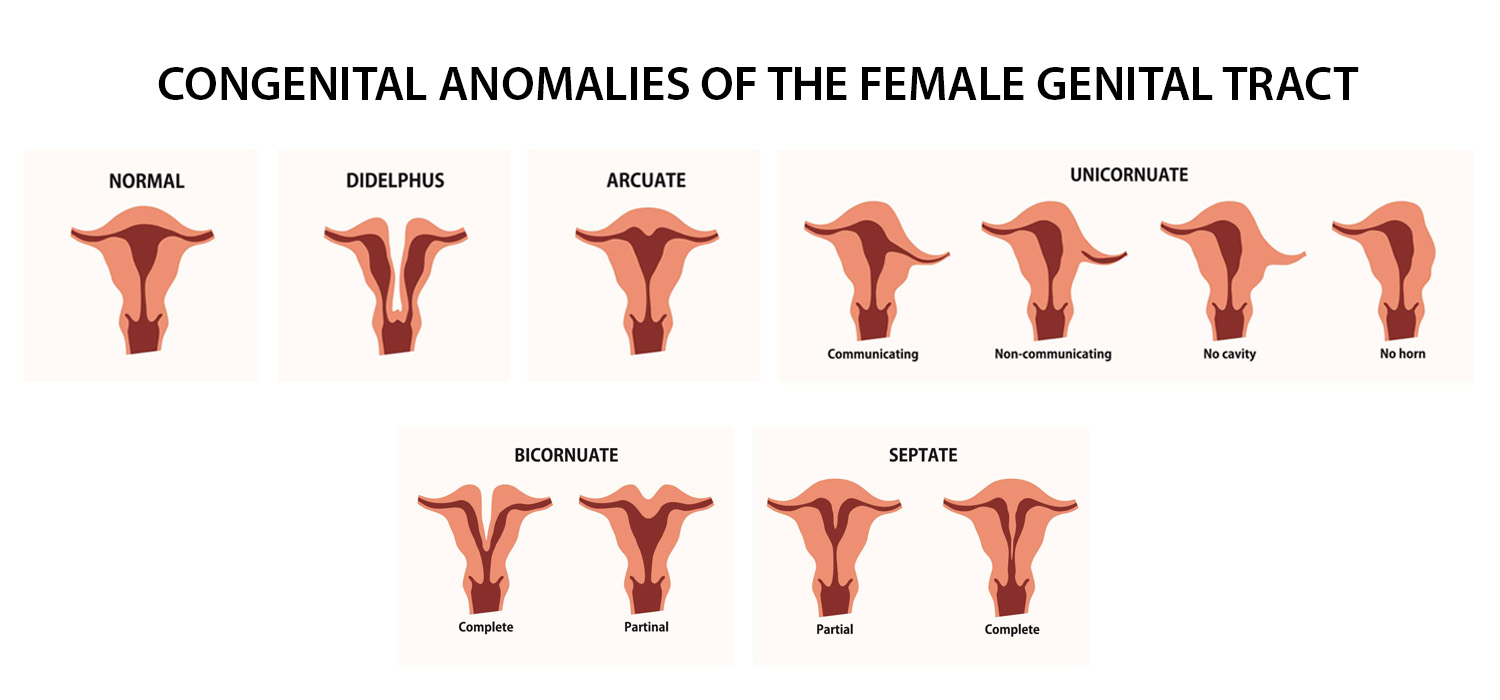
Classification of CUA
ASRM 2021 ( MAC 2021) classification
The anomalies are classified as total Mullerian agenesis, cervical agenesis, Unicornuate uterus, Uterus didelphys with longitudinal septum of variable length, bicornuate uterus, septate uterus, longitudinal vaginal septum, transverse vaginal septum and complex anomalies.
Ref Link: www.asrm.org/asrm-academy/asrm-academy-on-the-go/asrm-mac-tool/mac-tool/
ESHRE /ESGE classification (2013/2016)
Uterine, cervical and vaginal anomalies are classified and denoted with with respective numericals.
PDF Link: www.eshre.eu/conuta
Clinical presentation and diagnostic modalities
Most women with CUA are asymptomatic. Women having cyclic and non-cyclical pelvic pain might have an obstructive anomaly and must be differentiated from endometriosis. However endometriosis maybe also be present with uterine abnormalities. Septate and didelphic uterus can manifest as AUB while primary amenorrhoea is a feature of RMKH syndrome (Rokitansky Muller Kuster Hauser syndrome). CUAs can present as infertility also.
MRI is the gold standard for the diagnosis of CUA. 3D ultrasound along with SIS (Sono Infusion Sonography) or HSG can also be used for diagnosis when MRI is unavailable.
Reproductive outcomes in CUA
There is a reduction, though not significant, in the probability of achieving pregnancy in natural and ART cycles. Women with CUA are at an increased risk of preterm birth and second trimester miscarriages. Septate and bicornuate uterus are associated with increased miscarriage even in the first trimester. The effect of arcuate, didelphic and uni-cornuate uterus on reproduction is not statistically significant.
Management of CUA
Management of CUA depends on the type of abnormality.
Unicornuate uterus
A cavitary horn merits resection. Even the non-communicating cavitary horn must be resected as it is prone for endometriosis, ectopic pregnancy, dysmenorrhea and hematometra. A communicating cavitary horn merits resection. However, surgery is not recommended for non-cavitary, non- communicating horn.
Uterus didelphys
Metroplasty may be considered.
Women with Mullerian agenesis
(MRKH syndrome) are offered IVF with self eggs and surrogacy.
These women need psycho-sociosexual counselling and creation of neo vagina by Modified Abbe-McIndoe procedure or laparoscopic Verchietti procedure or laparoscopic creation of neo-vagina with ileal loop.
Bicornuate uterus
Surgery is not indicated if both horns are well developed. In 75-90% of cases, the rudimentary horn is non-communicating and need not be removed. When one horn is normal and the other is atretic, pregnancy is encouraged in the normal horn (By IUI/OI/ET) and an IUCD can be inserted in the rudimentary horn. When there is hematometra/pregnancy in the non-communicating horn, excision of the horn or unification after evacuation can be considered. Lap metroplasty can be considered for women with recurrent poor reproductive outcomes.
Bicornuate uterus
Surgery is not indicated if both horns are well developed. In 75-90% of cases, the rudimentary horn is non-communicating and need not be removed. When one horn is normal and the other is atretic, pregnancy is encouraged in the normal horn (By IUI/OI/ET) and an IUCD can be inserted in the rudimentary horn. When there is hematometra/pregnancy in the non-communicating horn, excision of the horn or unification after evacuation can be considered. Lap metroplasty can be considered for women with recurrent poor reproductive outcomes.
Septate uterus
Treatment of septate uterus, diagnosed incidentally, is debatable and unproven (RCOG).In patients with recurrent pregnancy loss, septal resection reduces miscarriage rates and improves live birth rate and can be offered to them.
T shaped uterus
Hysteroscopic metroplasty with incision on lateral uterine wall helps to expand the cavity.
For more info, Visit : www.medlineacademics.com