Role of genetics in male infertility
Genetic abnormalities may be encountered in 15-30% of male infertility.
The range of abnormalities is from varying degrees of oligospermia to azoospermia. There is a 20% chance of encountering genetic abnormality in men with these semen abnormalities.
What are the genetic abnormalities that may be encountered in male infertility?
Various genetic abnormalities that are encountered include:
- Aneuploidies
- Structural abnormalities like translocation and deletions
- X-linked and mitochondrial disorders
- Polymorphisms
- Autosomal gene Mutations
- Epigenetics and imprinting disorders
1) Aneuploidies in male infertility
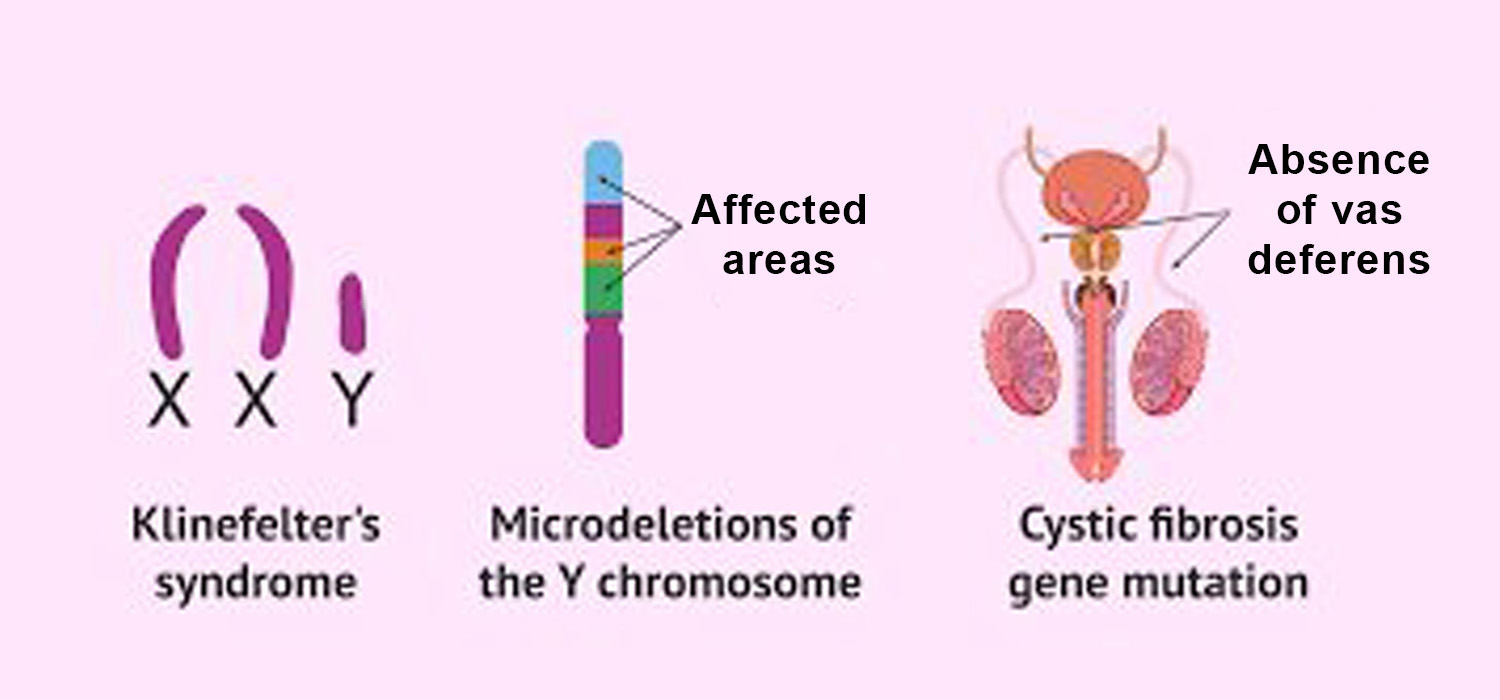
Men with non-obstructive azoospermia have greater incidence of aneuploidies esp of the sex chromosome eg. 47XXY
47 XXY aneuploidy – Klinefelter’s syndrome
The extra X chromosome is due to non-dysgenesis from mother or father. It is encountered in 5% of severe oligospermia cases and in 10 % of azoospermia cases. 90% of these are non-mosaics while 10 % of mosaic Klinefelter’s exist. FSH and LH are raised while the testosterone is reduced. Biopsy of the testes reveals germ cell degeneration.
In the mosaics, the sperms have 23X and 23 Y configuration.. The couple merit ICSI and since there is a risk of transmission to new born PGT is indicated.
47 XYY
The incidence in 1:0000 and the presentation is seen with severe oligospermia or azoospermia. The extra Y chromosome is due to abnormal meiotic pairing which results in sperm apoptosis causing oligo or azoospermia.
2) Structural abnormalities in male infertility - (A)Translocations
1) Balanced reciprocal translocation
Autosomal translocations are 4-10 time more common in infertile men than the normal men. The new chromosome is called the derivative chromosome. Since no genetic material is lost, there are no obvius chromosomal abnormalities.
2) Robertsonian Translocation (RT)
Prevalence of Robertsonian translocation is in infertile men is 9 times more than in normal population. Genetic material translocate from one to the other non-homologous chromosome. It occurs in acrocentric chromosomes- 13, 14, 21. The derivative gene is composed of two long arms while the short arm bits are lost. Though Robertsonian carriers are healthy , it can cause subfertility, infertility, miscarriage and chromosomal aberrations in the off-spring. Male carriers of RT of chromosome 21 have disomic gametes that can produce embryis with Trisomy 21.
3) Structural abnormalities in male infertility- (B) Y chromosome microdeletions
Y chromosome contains male specific genes necessary for spermatogenesis and steroidogenesis. Denovo deletion of the entire chromosome can cause 45XO or mosaics with 45X/46XY.
27 such genes have been identifies as necessary for the male functions.( 9 in short arm and 18 in long arm) The important ones are:
- AZF gene ( Azoospermia factor)
Includes AZF-a, AZF-b, AZF-C genes . The first two are responsible for spermatogenesis while AFZ-C is important for completion of maturation. AZF-a region has two important genes -USP 94 and DBY. Absence of both these results in Sertoli Cell Only syndrome. - DAZ gene ( deleted in azoospermia gene)
It has 4 copies and is involved in all stages of spermatogenesis. Clinically it results in a spectrum from oligo to azoospermia.
4) Autosomal gene mutations in male infertility
- CBAVD – Congenital bilateral absence of Vas deferens. This occurs due to mutation of CFTR ( Cystic fibrosis transmembrane conductance ) gene located on chromosome 7.
- Shortening of SHBG gene on Chromosome 17 can cause increased spermatogenesis with increased spermcount.
5) Gene Polymorphism in male infertility
Polymorphism implies the presence of more than two variant forms of a specific DNA sequence that can occur amongst different individuals.
Single Nucleotide Polymorphism (SNP) is the commonest form. Some polymorphisms that may impact infertility include:
- • FSH receptor gene polymorphism ( Chromosome 2)-Impacts spermatogenesis
- • ESR 1 & 2 genes ( Chromosome 6)- Reduced spermatogenesis
- • MTHFR gene polymorphism affects Folic acid synthesis, DNA methylation & spermatogenesis
- • INSL-3 gene ( Chromosome 19 ) & LGR 8 ( Chromosome 13) linked to Cryptorchidism
- • INSL-3 gene also implicated in testicular cancer, dysgenesis, hypospadiasis and infertility
6) X-linked gene disorders in male infertility
- AR gene on long arm of X-chromosomeis involved in spermatogenesis. Mutations can cause oligoasthenospermia, AIS, Kennedy syndrome ( neurogenetic disorder+abnormal spermatogenesis.
- Kallman’s syndrome-Has both X-linked and autosomal inheritance. It is characterised by hypogonadotropic hypogonadism with or without anosmia. KAL1 gene (short arm of Chromosome X ) deletions occur in 30-70% of KS patients. FGFR1 mutation ( Chromosome 8) causes anosmic Kallmann’s syndrome.
7) Epigenetic errors and male infertility
Imprinting is the last phase of spermatogenesis when methylation occurs to determine which paternal genes are expressed in the embryo. Hence the use of immature sperms in ART can result in ill established epigenetic code and the off-spring may have imprinting disorders.
New imprints occur in germ s=cells by reset of paternal imprints in every cycle. Normally paternal DMR (differentially methylated regions) are methylated and maternal DMRs are unmethylated. Patients with abnormal imprints have oligospermia, reduced success with ART, and increased risk of transmitting errors to off-spring.
8) Other genetic defects in male infertility
Impairment of mitochondrial DNA can cause abnormal spermatogenesis and over fifty Mendelian disorders can be associated with male infertility.
Hence it is important to bear in mind that oligospermia and non-obstructive azoospermia may also be associated with genetic disorders as enumerated above. Also ART may be less successful in men with genetic defects. Even with ART procedures there exists the risk of transmission of the same genetic defect to the male offspring. The couple must be counselled accordingly.
For more info, Visit : www.medlineacademics.com