Tubal Factors in infertility-Evaluation of the tubes
We shall discuss the various methods being used to evaluate tubal patency.
- Ultrasound Evaluation of the tubes
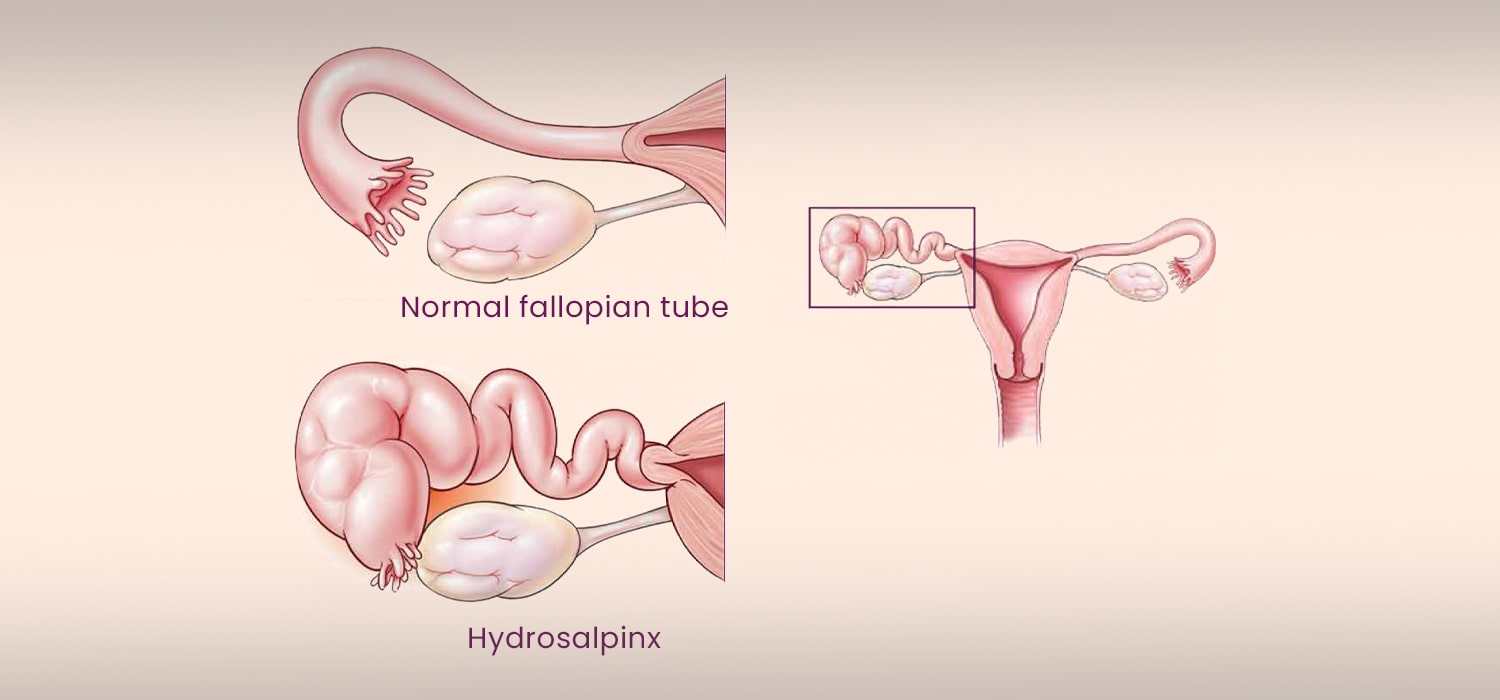
Normal tubes are not visualized on 2D or 3D scans unless there is fluid within or surrounding the tubes. Distended tubes on ultrasound are:- Thin or thick walled (in chronic cases)
- Elongated or folded appearing as tubular/retort shaped fluid filled structure.
- It is visualized as being separate from the uterus and ovary.
Cog-wheel appearance on scan is due to thickened, longitudinal folds of hydrosalpinx, seen on cross section and is pathognomonic of the pathology. Atypical hydrosalpinx without pseudo septations can be mistaken for an ovarian cyst. Densely adherent tubes which are thick and multiloculated can be mistaken for complex ovarian cyst. - Tubal patency tests (TPT)
The first step in performing TPTs is evaluation and treatment of any pelvic infection.
CDC control and prevention criteria to diagnose and manage PID out to be followed. No single test or symptom is diagnostic of salpingitis/ Though Laparoscopy is the gold standard in diagnosis of PID, there may be no evidence of salpingitis in 20% of cases. Treatment of PID appropriately is recommended. Similarly, Chlamydia antibody testing and testing for TB ought to be carried out before doing any tests for tubal patency.
The second step is the actual performance of tubal patency.- HSG and HyCoSy are screening tests for tubal patency and if positive for blockage, they must be followed up by laparoscopy, with or without hysteroscopy.
- Falloposcopy is hysteroscopic proximal tube examination using a flexible micro-endoscope of 0.5mm diameter, 1.73 mm long at 50X magnification and guided catheterization.
- Salpingoscopy is for endoscopic visualization of the distal tubal lumen by laparoscopy. A conical obturator helps the distal end of the sheath to enter the tubal ostium.
- HSG
It is an inexpensive and widely available screening to assess uni-or bi-lateral blockage of the tubes providing a permanent visual record. 10ml of water-soluble radio-contrast is instilled transcervically and serial X-rays are taken of the pelvic cavity. The low accuracy of the test is often due to cornual spasm. Gentle handling and administration of anti-spasmodic injection or tablet before the procedure helps overcome this spasm. HSG is contra-indicated during pregnancy and in the presence of PID. Hence it is done in the late follicular phase, around D7-12 of the menstrual cycle. The radiation exposure is around 0.4-5.5mGy. Performing HSG with oil-based dye has been shown to give better pregnancy rates. But water-based dyes are preferred because of better image quality and safety.
HSG is a reliable indicator of tubal patency if spill is seen on both the sides. However, it has a low sensitivity of 53-65% but a high specificity of 83-87%. It helps predict proximal tubal blockage and hydrosalpinx with moderate accuracy but is inaccurate in the diagnosis of or ruling out distal tubal obstruction or peri tubal adhesions.
Advanced HSG may be done with fluoroscopic guidance, manipulation, tubal cannulation, and tubal pressure to yield more information and reliability of testing. This is categorized as:
Category 1: Normal, good chances of future fertility. Very low incidence of ectopic pregnancy
Category 2: Patent tubes with tubal disease. 2a-Mild tubal disease, 2b-moderate tubal disease. These have moderate prognosis and outcome for future fertility and also highest incidence of ectopic pregnancy.
Category 3: Patent or blocked tubes with severe tubal disease. They are ideal for ART and have a low incidence of ectopic pregnancy. - SSTC (Selective salpingography and tubal catheterization)
This is ultrasound or hysteroscopy guided tubal cannulation done to identify and tackle proximal tubal occlusion. - Sonohysterosalpingography
This is done to determine tubal patency using transcervical fluid instillation, the filling and flow is monitored by transvaginal ultrasound. The two common methods that are used are Sion’s test or SIS and HyCoSy. Though fluid can be noted in the pouch of Douglas with saline infusion, the test does not differentiate between unilateral or bi-lateral patency.
Use of 3D ultrasound and color or power Doppler for sonographic visualization of insufflated tubes helps to identify tubal and uterine factors clearly.
Sonohysterosalpingography is a better alternative to HSG as it has higher sensitivity (76%-96%) and specificity (67-100%) - Tubal insufflation ( Rubin’s test)
Air or carbon-di-oxide is pushed into the uterus transcervically. Hissing sound on auscultating the iliac fossa and shoulder tip pain are suggestive of tubal patency. However, it is no longer performed as it is very subjective, unreliable and cannot be documented. - Transvaginal hydrolaparoscopy (THL) and Fertiloscopy:
THL involves small diameter endoscopic visualization of the pelvis after instillation of 500 ml of fluid instilled through a needle inserted in the posterior vaginal fornix.
When hysteroscopy, falloposcopy and distal tubal salpingoscopy are done along with THL, it is termed as fertiloscopy. This can be done as an OPD procedure under local anesthesia. Minor adhesiolysis, endometriosis fulguration etc may be performed concurrently. The findings are almost similar to laparoscopy findings and are reliable. However, the risk of bowel injury is much higher when compared to laparoscopy and THL is not useful in evaluating women with obliterated POD.
For more info, Visit : www.medlineacademics.com