PPOS (Progesterone Primed Ovarian Stimulation)
PPOS has emerged as a revolutionizing protocol in infertility treatment. It is a new ovarian stimulation protocol that can block the luteinizing hormone (LH) surge by using progesterone instead of the traditional downregulation using GnRH agonist or antagonist in controlled ovarian stimulation cycles.
Premature LH surge is a major cause for cycle cancellation during ovarian stimulation in women undergoing IVF and occurs in 20-25% of conventional stimulation cycles.
Mode of action of Progestins in causing pituitary suppression:
Though progesterone is the key signal in the mid cycle dynamics, the exact mechanism through which progesterone interacts with estradiol to regulate the LH surge is not known.
Facts known about progesterone.
Endogenous progesterone could hinder the rise of LH resulting in no spontaneous LH surge during controlled ovarian stimulation.
Progestins reduces GnRH’s pulsatility from the hypothalamus, thus inhibiting the release of LH that occurs with increasing estradiol levels.
Why was PPOS not used previously?
As previously the emphasis and practice was of fresh embryo transfers, progesterone could not be considered for use during ovarian stimulation because it was known to have a negative impact on endometrial receptivity. However, with the advent of robust embryo cryopreservation techniques, and hence the transfers of frozen embryos, it has become feasible to use progestin as an alternative agent for the suppression of premature LH surge during ovarian stimulation.
Application of PPOS: PPOS can be routinely used. However,
- It helps to enhance the sensitivity of the ovaries to gonadotropins, potentially improving the quality and number of retrieved oocytes.
- It prevents OHSS.
- It ethe enhances endometrial receptivity.
Protocols of PPOS
The progestins most often used is Medroxyprogesterone in the doses of 10-20 mgs daily. Usage of Dydrogesterone has been documented with similar results. Dydrogesterone has been shown to exhibit no or weak inhibition of ovulation at a normal dosage and can be an adjuvant to hMG during ovarian stimulation.
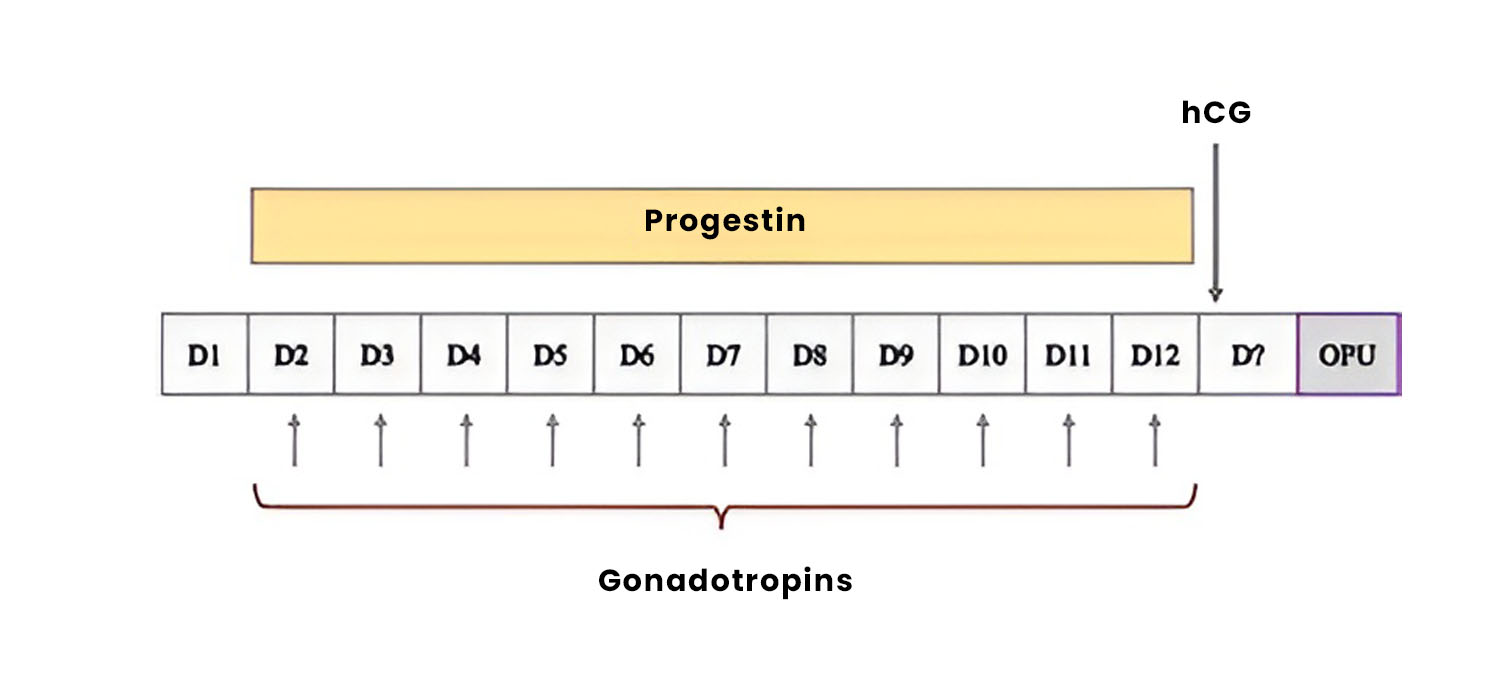
In the fixed Progestin PPOS, the progestins are started on day 2 of the menstrua cycle along with the gonadotropins.
In the flexible PPOS protocol, progestins are started when a follicle reaches 12 mm or when the estrogen levels are more than 200 pgms/ml, by day 5 of the cycle.
At times, in the modified natural cycle protocol, with the aim of minimum ovarian stimulation, progestin is introduced in the early follicular phase the gonadotrophins are added later in the cycle to support follicular development. This is for patients who wish to minimise the use of exogenous hormones.
Challenges with PPOS
While PPOS presents a promising advancement in infertility treatment it has its own challenges. The optimal dosage and timing of progestin administration are critical factors and individual patient responses may vary.
The potential impact of PPOS on pregnancy outcomes and the long-term health of offspring require further studies and follow-up.
Studies and Clinical evidence:
Several studies have reported improved oocyte quality, increased implantation rates and a reduction in the incidence of OHSS in patients undergoing PPOS compared to traditional stimulation protocols.
A multicentric randomised controlled trial comparing PPOS with the standard GnRH agonist protocol in poor responders found that PPOS resulted in higher oocyte retrieval rates and increased clinical pregnancy rates, thus highlighting its potential as a viable alternative for such challenging scenarios.
Studies focusing on patients at risk of OHSS demonstrated a significant reduction in the incidence of moderate to severe OHSS in those who underwent PCOS compared to a conventional antagonist protocol, thus mitigating the risks associated with ovarian hyperstimulation.
Studies have thus far also shown that use of projections in PPOS was a safe option for the newborn population without compromising neonatal outcomes or increasing congenital malformations.
SWOT analysis of PPOS:
Strengths - Well tolerated, low cost, comparable number and quality of oocytes, similar pregnancy rates and no incidence of OHSS.
Weakness - Fewer RCTs, need for freezing, increased dosage of gonadotropins.
Opportunities - number of euploid blastocysts, especially in poor responders, Dual stimulation possible, patient friendly because of easier scheduling of injections, random start of stimulation is possible.
Threats - Changes in current/ traditional practice, relies on robust Cryopreservation and subsequent frozen embryo transfer, limited data on obstetric and perinatal outcomes ( especially long term)
Future role of PPOS:
- Donor stimulation
- Fertility preservation
- PGT-A & PGT-M cycles
- Double ovarian stimulation and non-conventional protocols
To conclude progesterone primed ovarian stimulation represents a paradigm shift in infertility treatment offering a tailored approach for patients with unique challenges such as poor ovarian response or history of OHSS. The diverse protocols available allow for customisation of treatment plans and protocols, based on individual patient profiles and hence optimising the chances of success.