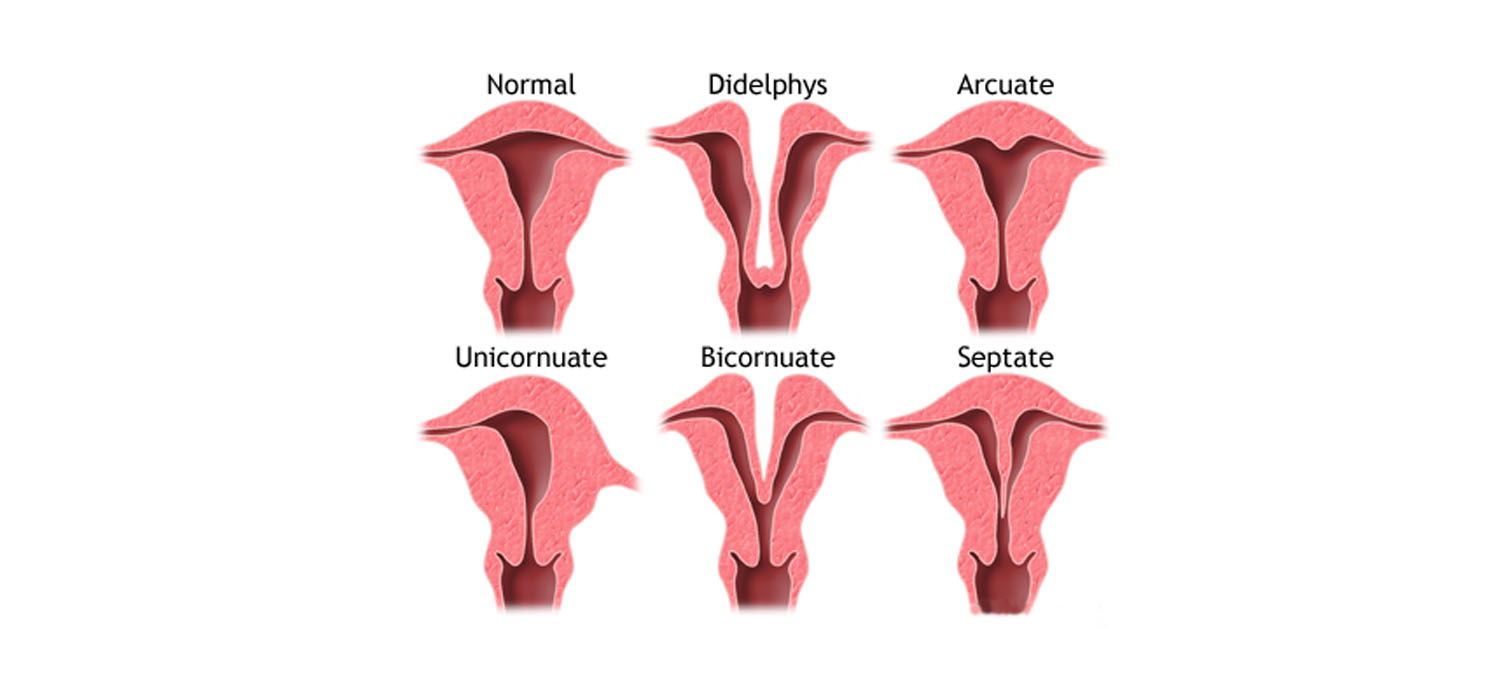
Management of congenital Uterine anomalies
The prevalence of congenital uterine anomalies in the general population is about 4.3-6.7%. IN the infertile population, it is reported to be about 3-13% and in patients with recurrent miscarriage, it is reported as 12.6-18.2%.
Reproductive outcomes in CUA
There is a reduction, though not significant, in the probability of achieving pregnancy in natural and ART cycles. Women with CUA are at an increased risk of preterm birth and second trimester miscarriages. Septate and bicornuate uterus are associated with increased miscarriage even in the first trimester. The effect of arcuate, didelphic and uni-cornuate uterus on reproduction is not statistically significant.
General principles in the management of anomalies:
- Management of CUA depends on the type of abnormality.
- An incidental finding with no effect on previous obstetric outcome may not necessarily need treatment.
- Minimally invasive surgery (MIS) in the form of endoscopic surgery-hysteroscopy- is often the first choice of surgical intervention.
Management of specific anomalies
- Unicornuate uterus
Uterine remnant with functional endometrium, on the other side of a unicornuate uterus merits resection. Even if it is non-communicating, the cavitary horn must be resected as it is prone for endometriosis, ectopic pregnancy, dysmenorrhea and hematometra. Similarly a communicating cavitary horn also2 merits resection. However, surgery is not recommended for non-cavitary, non- communicating horn. - Uterus didelphys - Metroplasty may be considered.
- Women with Mullerian agenesis
(MRKH syndrome) are offered IVF with self-eggs and surrogacy. These women also need psycho-sociosexual counselling and creation of neo vagina by Modified Abbe-McIndoe procedure or laparoscopic Verchietti procedure or laparoscopic creation of neo-vagina with ileal loop. - Bicornuate uterus
Surgery is not indicated if both horns are well developed. In most cases, the rudimentary horn is non-communicating and need not be removed. When one horn is normal and the other is atretic, pregnancy is encouraged in the normal horn, either by IUI or IVF.
IUCD can be inserted in the rudimentary horn.
When there is hematometra/pregnancy in the non-communicating horn, excision of the horn or unification after evacuation can be considered.
Lap metroplasty can be considered for women with recurrent poor reproductive outcomes. - Septate uterus
Treatment of septate uterus, diagnosed incidentally, is debatable and unproven (RCOG).
However, in patients with recurrent pregnancy loss, septal resection has shown to reduce miscarriage rates and improve live birth rate.
Hysteroscopic septolysis is the surgery of choice. - T shaped uterus
There exists no definite criteria for diagnosis of T-Shaped uterus. The ESHRE/ESGE has mentioned dysmorphic uterus (T-shaped) as one with narrow cavity and thick lateral wall without specifying the measurements for diagnosis. There is no mention in ASRM and the CUME has attempted to define it as:- Lateral indentation depth >/= 7mm
- Lateral Indentation angle
- T-angle
Hysteroscopic metroplasty with incision on lateral uterine wall helps to expand the cavity. However, it may well be that non-DES related T-shaped uterus cannot be regarded as an anomaly and may not merit treatment.
Thus the treatment of uterine anomalies is tailor made to the type of anomaly and presentation. Minimally invasive endoscopic interventions are the surgeries of choice.