PCOS (Polycystic Ovarian Syndrome) and pregnancy
PCOS is a complex, heterogenous endocrine disorder, due to synergistic action of genetic, epigenetic and environmental factors associated with reproductive and metabolic disorders; resulting in short and lone term consequences on women’s health.
PCOS and infertility
There exists menstrual disorder and inefficient / absent ovulation (release of eggs) in women with PCOS. Generally, anovulation is the cause of infertility in 30-40% of cases. But 80-90% of WHO category 2 ( Normogonadotropic/Normoestrogenic) cause of anovulation is due to PCOS.
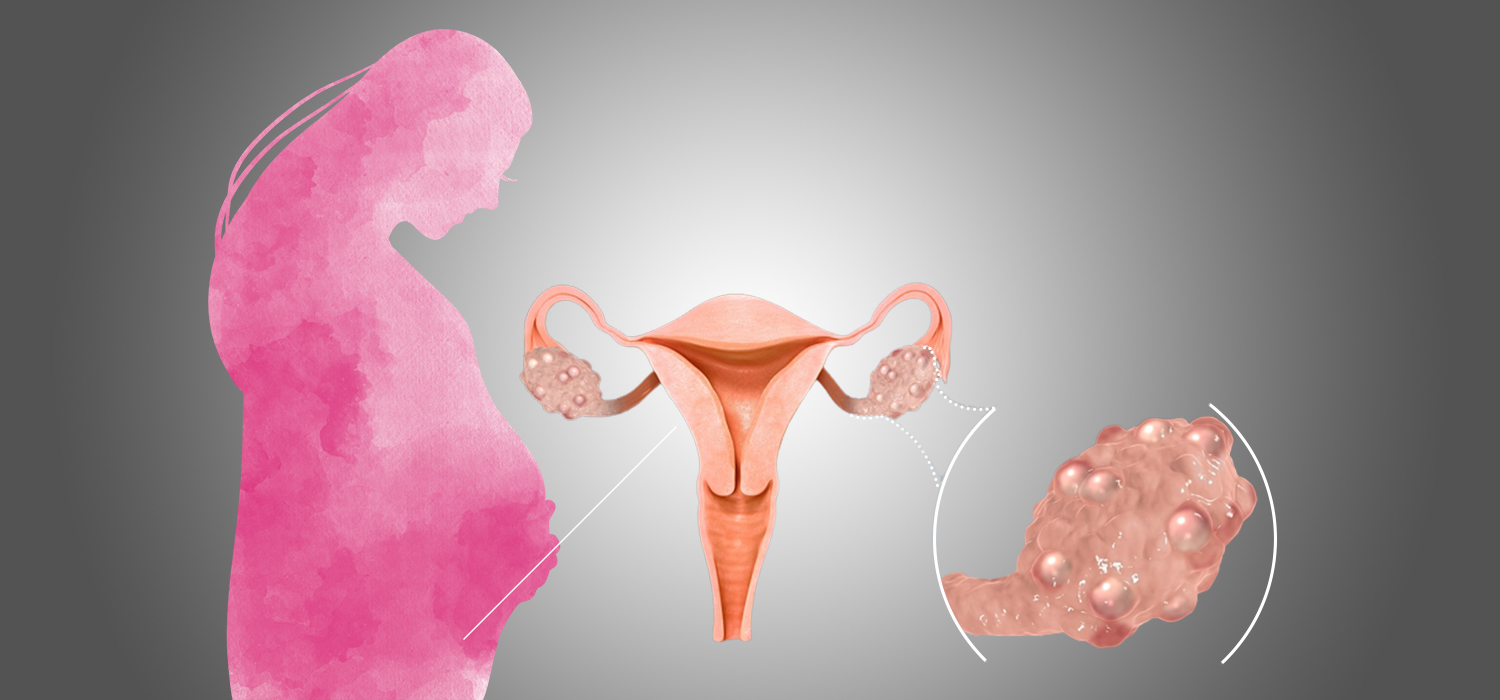
The features of PCOS include irregular menstrual cycle ( often delayed periods) and /or signs of excessive androgen ( Male hormone) secretion .This includes acne, hirsutism ( excess hair especially facial) and baldness. Visualizing the ovaries that appear large and show multiple small cyst of 2-9 mm with a thick central area helps in diagnosing PCOS.
As there exists impaired ovulation, women with PCOS may have difficulty in getting pregnant and often need medical intervention. Depending on other existing conditions and/or male factor infertility, the type of treatment may vary form oral medications to injectables, just advising timely intercourse with medications to offering IUI ( Intra Uterine Insemination) or other assisted reproductive techniques like IVF ( In Vitro Fertilization ) or ICSI (Intra Cytoplasmic Sperm Injection) with ET ( Embryo transfer)
Are pregnancies in PCOS patient considered high risk?
Yes. For various reasons.
When the woman has conceived after treatment or ART, the pregnancy is considered precious.
Also, any pregnancy – singleton or twins-in PCOS patients is associated with several risks both to the mother and the baby.
What are the causes of high risk in PCOS pregnancies.
There exist several causes. Increased androgens in circulation presence of impaired glucose tolerance( IGT) or even overt type 2 diabetes, obesity, presence of certain metabolic impairments like deranged lipid profile, hormones etc contribute to the risk. Many causes act synergistically to enhance their negative effect.
Abnormalities in egg development and release means poor quality of eggs and subsequently defective fertilization/ pregnancy.
What are the risks in PCOS-pregnancies and why?
- 1. Delay in conceiving. Many PCOS women may need several cycles of treatment before they get pregnant.
- 2. Increased risk of mis-carriage- 24-36%. This is due to obesity, defective folliculogenesis, hyperandrogenism, Insulin resistance, incompetent oocytes, altered leptin and endometrial receptivity.
- 3. Increased risk of recurrent pregnancy loss -36-56%. Recurrent pregnancy loss means repeated loss of pregnancy for 2-3 consecutive times.
- 4. Increased risk of medical disorders in pregnancy- Gestational diabetes, gestational hypertension
- 5. Increased neonatal complications- Small for gestational age babies with their attended complications, increased NICU admissions Presence of maternal obesity with/ without co-existing diabetes can result in a large for gestational age baby with its attended complication.
- 6. Obstetric complications include Shoulder dystocia which occurs in 2nd stage of labor due to a large baby or occu7rence of post-partal thromboembolism.
What precautions must be taken in order to avoid complication of PCOS-pregnancy.
Avoiding pregnancy complications starts well before getting pregnant!!
Pre-conceptional care is an important aspect for any women trying to conceive and especially so for those women with PCOS.
Women are advised to optimise their weight. The ideal BMI (Body mass Index) is 19-24 and women who are trying to conceive must conform to this. In fact, a 5-10% reduction of existing weight augurs well for women with PCOS who are obese/ over-weight. Sometimes, spontaneous conception, without using medications, can occur with weight reduction secondary to the right diet and exercise!
Folic acid supplementation. 4 mgs of folic acid 6-8 weeks before conceiving has been proven to prevent the occurrence of neural tubal defects like anencephaly and spinal defect like meningocele/ meningo-myelocele etc. For obese women the dose of folic acid is 5 mgms/ day.
Other lifestyle modifications include cessation of smoking and limiting alcohol consumption.
Women with recurrent pregnancy loss may merit evaluation of Serum homocysteine levels.
Metformin therapy helps to reduce weight, reduce insulin resistance and hyperinsulinemia, risk of diabetes and miscarriage. However there do not exist convincing evidence that metformin during or before pregnancy can reduce pregnancy complications and improve live birth rates.
Prevention of OHSS included:
Primary prevention- The woman’s risk for OHSS is assessed before the start of treatment and the stimulation protocols for ovarian induction is tailor made to her. This involves using lower doses of gonadotropins ( medication to induce ovulation) , changing the protocols, avoiding hCG injection for ovulation trigger and adding insulin sensitizing medications ( like Metformin) during stimulation.
Secondary Prevention: This involves identifying cases threatening to progress into OHSS and taking appropriate measure to reduce the risk and complication thereon. These measures may include using alternative medications for ovulation trigger (GnRH agonist or rLH) instead of hCG, reducing the dosage of hCG trigger, freezing (cryopreservation) all embryos and transferring it in an unstimulated cycle, using dopamine agonists (like Cabergoline) and using adjuvant medications like calcium infusion, steroids, aspirin etc.
To conclude…
PCOS is a heterogenous, complex endocrine disorder whose effects have ramifications throughout the lifespan of a woman.
The effects during pregnancy can be ameliorated by appropriate pre-pregnancy care as well as good antenatal care.
For more info, Follow : medlineacademics.com