OHSS (Ovarian hyperstimulation Syndrome)
What is OHSS?
It is a complication that can occur during ART (Assisted Reproductive Technology) process. It occurs due to the use of certain medications to stimulate egg production from the ovaries during ART.
Is it serious?
OHSS occurs as mild, moderate, severe, and even critical forms. Mild OHSS can occur in upto 30 % of women receiving ovulation induction in ART while the severe for can occur in 2-3% of IVF ( In Vitro Fertilization patients). Death due to OHSS can occur in one in 4.5 to 5 lakh cases.
Who are the women at risk of OHSS?
OHSS can occur in any woman who is receiving medication for induction of ovulation. However OHSs can be more common in younger women, women with PCOS ( Poly cystic ovarian syndrome) especially in lean PCOS, women with high ovarian reserve as evidenced by increased AMH ( anti Mullerian Hormone) levels and AFC ( Antral Follicle Count). Other risks during stimulation include increased number of follicles on the day of trigger ( over 14 follicles) and/or high and rapidly rising estrogen (E2) values ( E2 > 5000 ng/ml).
What is the cause of OHSS?
The signs and symptoms of OHSS result due to certain chemicals secreted in the body when the ovaries respond excessively during stimulation. These causative chemicals include hCG ( Human chorionic gonadotropin) which acts through VEGF ( Vascular Endothelial growth Factor), RAS ( Renin-Angiotensin System ) both at local ovarian level and at systemic level, while the end- mediators include Interleukins 1,2,6,8 ; Tumor necrosis factor alfa, Endothelins etc.
The final pathway is depletion of fluid from the intravascular space to the third compartment resulting in hemoconcentration and its attended complications, accumulation of fluid in the peritoneal, pericardial and pleural spaces ( causing ascites, pericardial effusion, pleural effusion), coagulation disorder (DIC and thrombosis) and also compromises the internal organs like Kidney and Liver.
Early OHSS develops because of administering hCG injection as a trigger for ovulation during treatment. Late OHSS is when it develops because the woman has conceived in the treatment cycle. (Hence embryo transfer resulting in possible pregnancy is deferred in an IVF cycle with risk/ possibility/ evidence of OHSS)
What are the signs and symptoms of OHSS?
A woman undergoing ART undergoing ovarian stimulation can present with:
Abdominal pain, bloating, thirst, nausea vomiting, difficulty in breathing (dyspnea) and reduced or absent urinary output, in severe cases.
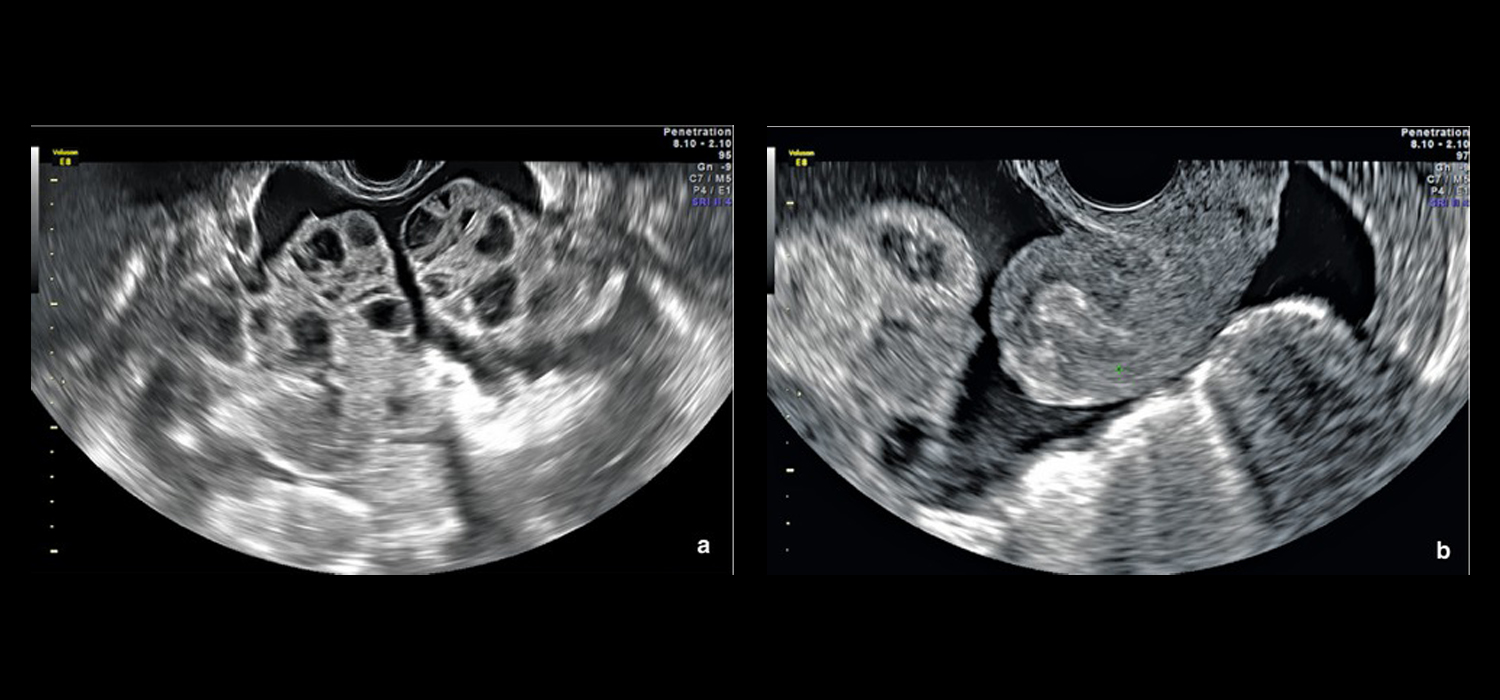
Ultrasound shows evidence of enlarged cystic ovaries and accumulation of fluid within the abdominal cavity. Blood examination revels evidence of hemoconcentration (raised hematocrit, raised WBC count), impaired renal and liver function test, impaired coagulation profile.
Depending on the degree of clinical symptoms and signs; and the laboratory and ultrasound parameters, OHSS can be grouped as mild, moderate, severe and critical.
Can OHSS be prevented?
Yes!!
Prevention of OHSS included:
Primary prevention- The woman’s risk for OHSS is assessed before the start of treatment and the stimulation protocols for ovarian induction is tailor made to her. This involves using lower doses of gonadotropins ( medication to induce ovulation) , changing the protocols, avoiding hCG injection for ovulation trigger and adding insulin sensitizing medications ( like Metformin) during stimulation.
Secondary Prevention: This involves identifying cases threatening to progress into OHSS and taking appropriate measure to reduce the risk and complication thereon. These measures may include using alternative medications for ovulation trigger (GnRH agonist or rLH) instead of hCG, reducing the dosage of hCG trigger, freezing (cryopreservation) all embryos and transferring it in an unstimulated cycle, using dopamine agonists (like Cabergoline) and using adjuvant medications like calcium infusion, steroids, aspirin etc.
What is OHSS-free clinic?
Anovulation (non-production of eggs) is managed by giving the woman medications to induce ovulation . This is monitored by serial ultrasound and an injection for triggering Ovulation at an appropriate time.
Antibiotics for infections that may be causing tubal/ Peritoneal factors, release of adhesions in the pelvis by performing laparoscopy. Removal of polyps and fibroids implicated in causation can be removed by hysteroscopy and/or laparoscopy.
Unexplained infertility mandates further investigations and tailor-made strategies to manage the couple.
To Conclude….
World over, there is an inclination to not just reduce the incidence of OHSS but to keep the ART treatment completely free of OHSS.
This involves a segmentation approach:
Segment A- Optimization of Ovarian stimulation. Using GnRHa trigger in GnRH Antagonist protocol.
Segment B- Optimization of cryopreservation of oocyte/ embryo. Freeze all.
Segment C- Optimization of endometrial implantation potential. Embryo transfer in an unstimulated cycle with a receptive endometrium ( natural or artificially prepared)
How is OHSS managed?
OHSS is a self-limiting condition. There do not exist any specific treatment measures.
Secondary prevention, early recognition and symptomatic/ supportive treatment is the main stay of treatment.
Mild and moderate cases do not require hospitalization. However, the patient must be made aware of the condition. She must avoid intense exercises and sexual intercourse. Her fluid intake is guided by thirst and her weight, abdominal girth and vital parameters must be measured daily. An intake and output chart must also be maintained. Analgesics like paracetamol or opioids may have to be given , NSAIDs are best avoided. Monitoring should continue till symptoms abate or the patient gets her menses.
Severe and critical OHSS merit hospital admission. Admission is also indicated if the symptoms worsen during domiciliary treatment, or the patient is uncompliant or has unsatisfactory pain control.
Management includes IV fluids to correct hydration and dyselectrolytemia, appropriate analgesics for pain relief, anticoagulants to prevent thromboembolic episodes. Monitoring of vitals, fluid input and urine output charts are mandatory. Blood tests include full blood count / hematocrit, liver and renal functions, electrolytes and coagulation profile.
Paracentesis (removal of fluid from abdominal cavity) may be indicated in tense ascites, oliguria, hemoconcentration not responding to medical therapy, shortness of breath due to increased abdominal pressure.
Surgical management is warranted in cases of adnexal torsion, ectopic pregnancy, ovarian rupture, or hemorrhage.
To conclude,
OHSS is a threat to any patient undergoing ovarian stimulation. Efforts are being made earnestly to ensure an OHS- free clinic by optimizing ovarian stimulation, embryo/oocyte freezing and resorting to frozen embryo transfer in subsequent cycles.
For more info, Follow : medlineacademics.com