Morphological assessment of Oocyte and embryo
It is indeed a marvel of modern science that we can retrieve the eggs for fertilization outside the human body, and later implant the embryo with the uterus. But,
What is the need to assess the oocyte after pickup or the embryo after fertilization?
It is obvious that we expect the best outcomes and for this a best quality oocyte and embryo is a pre-requisite. Despite advances there is no fool=proof method of selecting the best embryo for implantation. Morphological assessment and grading of the embryo is the most commonly applied method for selection as it is non-invasive, needs no extra instruments, is not time consuming and most often, if not always, correlates with outcome.
Advanced methods of assessing embryo quality include Time Lapse monitoring, proteomics, and genetic testing of embryos.
How are oocytes assessed?
After the LH surge the oocytes resume meiosis. From the arrested diplotene stage of Prophase I, they progress and reach the metaphase of Meiosis II and hence termed as MII oocytes.
After the oocyte retrieval, the oocyte is categorized as mature, immature, post-mature or atretic depending on the cellular investments around it.
A mature oocyte is spherical and around 120-micron meter and surrounded by a zona pellucida (ZP)which is a matrix of three intermediate filament proteins ZP1, ZP2 and ZP3. The cytoplasm of a healthy oocyte, called as oolemma, is translucent with evenly distributed granularity. It contains mitochondria, peroxisomes, endoplasmic reticulum, Golgi complex, vacuoles, and other organelles. The peri-vitelline space is the space between oolemma and the ZP and houses the polar body. The (first) polar body is the product of continuing meiosis, extruded at ovulation while the second polar body is extruded at fertilization. A healthy oocyte has a spherical or round polar body. The presence of vacuoles, refractile bodies, smooth endoplasmic reticulum, mitotic spindle (visualized with polarized microscopy) is also looked for.
Assessment of fertilization.
The first assessment after ICSI is after 16-18 hours to assess the fertilization. The resultant embryo is said to be in the pro-nuclear stage. The key parameters that are monitored include the size and symmetry of the two pro-nuclei (maternal and paternal), the number, size and distribution of the nucleoli and the cytoplasmic appearance. The presence of two fully formed pro-nuclei, two polar bodies and an intact ZP is an indicator of proper fertilization. Pronuclear morphology is considered an indicator of embryo development.
Evaluation of embryos.
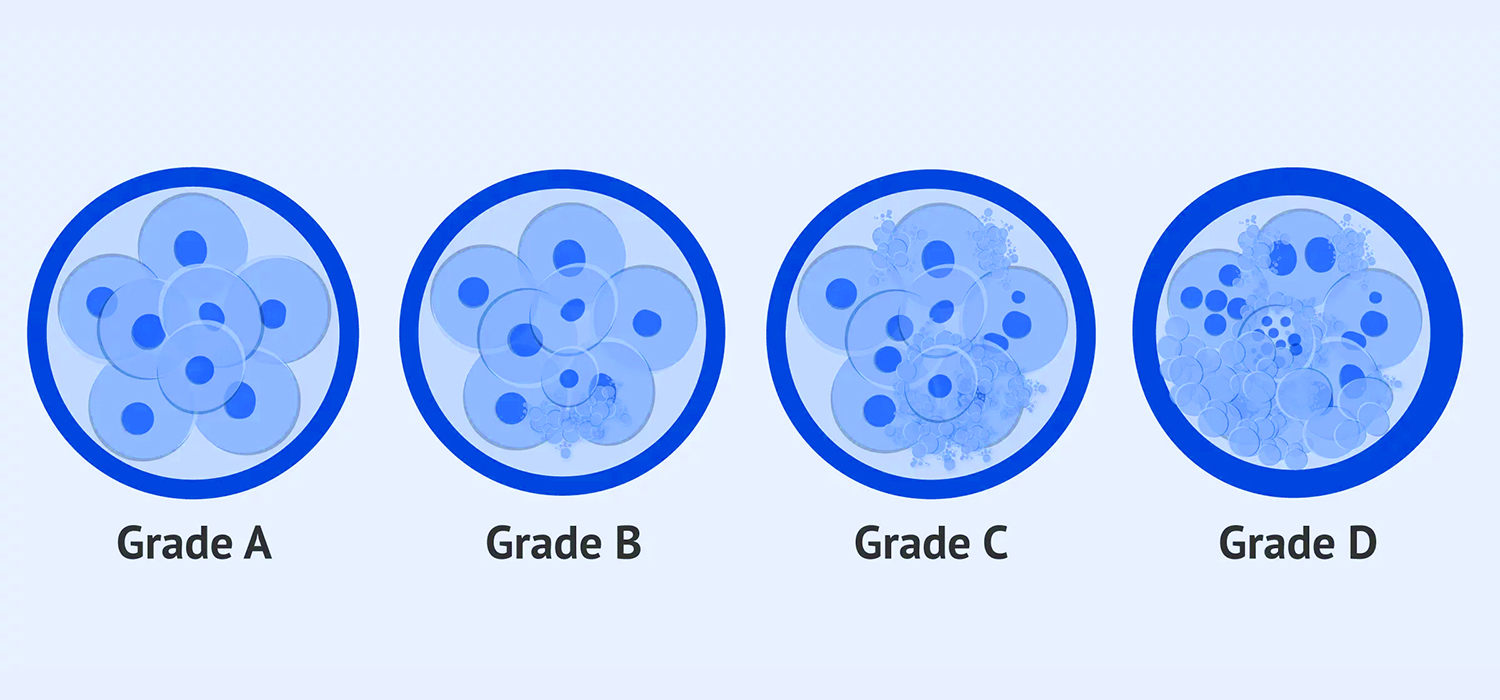
After successful fertilization, embryos are evaluated at the cleavage stage, which is Day 3 and later at D5- that is the blastocyst stage. At 68 +/- 1 hour, a healthy embryo has 6-8 equally sized, mononucleated, blastomeres and the cytoplasm has no or less than 10% fragmentation. These are grade I embryos. The grade II and Grade III embryos have >15% and >50% fragmentation. The grade III is not selected for transfer.
The embryo on Day 5 is a blastocyst and can be evaluated on the basis of the amount of blastocele fluid, Inner cell mass (ICM) and the outer trophoblastic layer. An expanded blastocyst with thin ZP, blastocoel filling almost the entire area, sickle shaped trophectoderm and a tightly packed inner-cell mass comprising about 25% of blastocoel merits to be certified as Garde I (1AA).
Are there other ways to assess morphology?
Time Lapse Imaging is an advanced technique where images of embryos taken at different timings can be studied for progress or otherwise without disturbing the microenvironment. This system can indicate the embryos which are displaying ideal growth pattern but cannot indicate that the other embryos are incapable of initiating pregnancy.
Metabolomics and proteomics are advanced studies that aim to assess the functioning of a ‘normal’ growing embryo. Study of the culture media in which the embryos have been cultured, study of blastocele fluid are some of the advanced methods which aim to ascertain normal functioning for better outcomes.
Finally, it is important to note that morphologically normal embryos may also implant poorly while slightly substandard embryos can implant satisfactorily and continue to grow.
For more info, Follow : medlineacademics.com