Monitoring of Ovarian stimulation - Part 2
Ultrasound Monitoring of Ovarian stimulation
Ultrasound is quick, easy, non-invasive and not harmful to the oocyte. The transvaginal scan is preferred and the technique has been validated under normal,anovulatory and gonadotropin stimulated conditions.
Base line scan is done on the 2nd or 3rd day of menstrual cycle. The AFC ( Antral Follicle Count-number of 2-9 mm follicles) categorizes patients as normal, poor and hyper-responders. A low AFC of 3-6 follicles is associated with poor response to ovarian stimulation but does not predict failure to conceive. AFC of over 14 follicles predicts hypersensitivity with 82% sensitivity and 89% specificity.
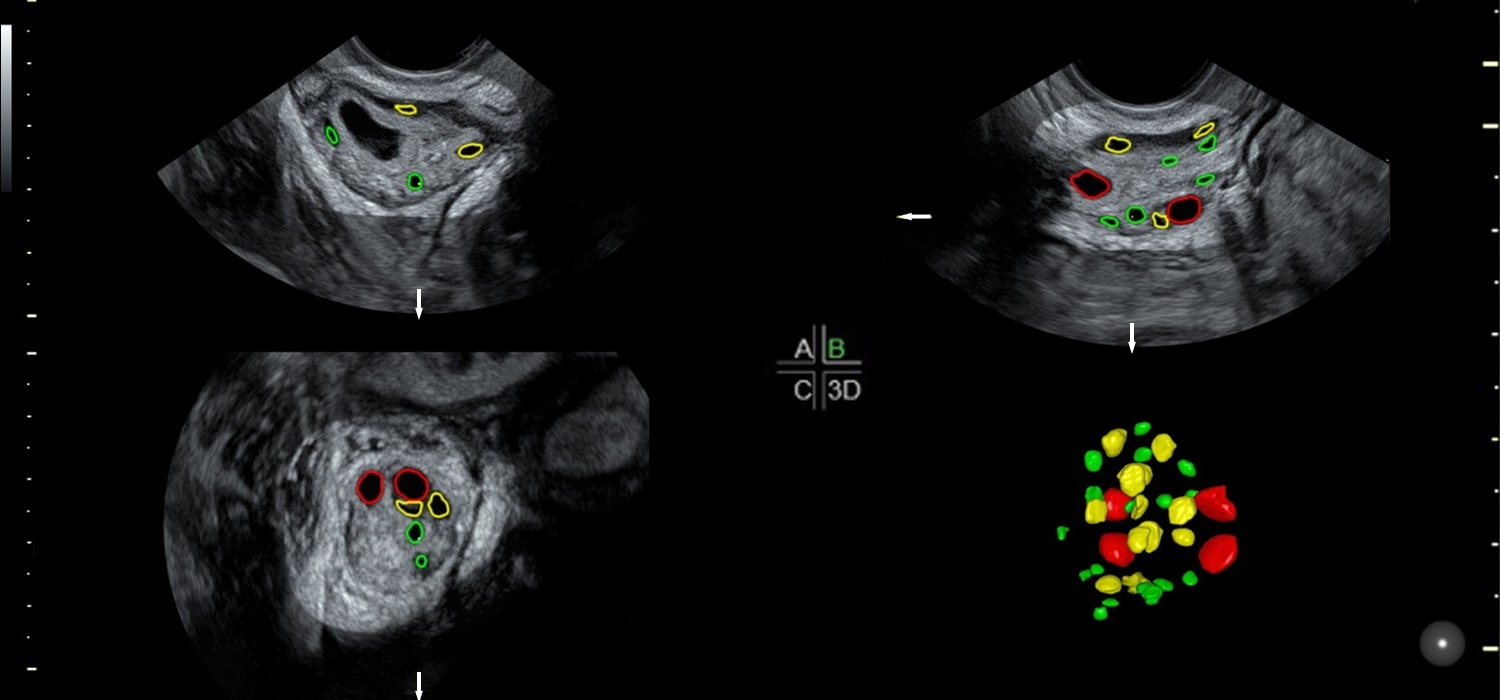
3D ultrasound may be performed manually through VOCAL ( Virtual Organ Computer Aided Analysis) or automated by using SonoAVC (Sonography based automated volume calculation) Poor response to stimulation is predicted when volume is < 3mL with specificity of 80-90% and sensitivity of 11-80%.
Intraovarian flow indices
Ovarian blood flow can be calculated at the start of the cycle and correlates well with subsequent follicular development in IVF cycles. There appears a good correlation between ovarian stromal flow index (FI) and number of mature oocytes retrieved and also with pregnancy rates in IVF cycles.
Stromal Peak Systolic Velocity (PSV)<10 after pituitary suppression is indicative of poor response.Stromal PSV>10 with unchanging resistance predicts risk of hyperresponse.
Uterine artery flow indices - Uterine artery resistance index (RI) > 0.79 is associated with poor response and thus can predict the need for higher doses of gonadotropins. Lower uterine RI and higher PSV predicts OHSS.
Monitoring during stimulation
This includes follicular growth and endometrial thickness patterns.
The fate of follicle can be decided by size, growth rate ( >2-3 mms/day in conception cycle), wall thickness and internal echogenicity.
Prediction of ovulation is by increase in size, increasing granulosa thickness ( growth rate 2-3mm/day), cumulus-like shadow 36 hours prior to ovulation, sonolucent halo 24 hours prior to ovulation, separation and folding of follicle lining 6-10 hours before ovulation. Follicular growth pattern rather than follicular diameter has predictive value of oocyte quality. But it is difficult to assess during superovulation.
Perifollicular blood flow (PFBF)
PFBF indices are closely related to intrafollicular oxygen content and VEGF (Vascular Endothelial Growth Factor) concentration. Hence qualitative and quantitative analysis of PFBF by color doppler and power doppler can indicate follicular competence. 2 days prior to ovulation, the RI begins to fall and is lowest at ovulation and remains low for the following 4 days and begins to rise to 0.5 by mid-luteal phase.
Peri-follicular blood flow can be graded depending on the percentage of blood flow around a follicle. Grade 1 signifies blood flow to less than 25% of follicle circumference while Grade 4 implies blood flow to over 75 % of follicle circumference. A follicle with grade 4 PFBF with stromal PSV >10cms/sec and RI < 0.4-0.48 usually contains a good oocyte. PSV < 10cms/sec indicates high probability of developing into an abnormal embryo.
Ovarian Volume assessment by 3D
Ovarian volume is assessed along with doppler, vascularization of cumulus, perifollicular vascularization index (VI), Flow index (FI) and vascularization flow index (VFI). 3D ultrasound is more accurate in assessing follicular volume. Follicular volumes between 3-7ml ( Follicular diameter 12-24 mm) associated with better oocyte recovery rate, fertilization rate and cleavage rate.
Confirmation of ovulation
Disappearance of dominant follicle, reduction in size of follicle, irregular follicular contour, echoes within the follicle, corpus luteum formation, fluid in POD and hyperechogenic secretory endometrium suggest ovulation.
Doppler of the Corpus luteum
Doppler of the corpus luteum indicates functionality of corpus luteum. Normally the RI is 0.35-).5. But in LPD ( Luteal phase deficiency) RI is 0.54-0.62, PI is 0.7-0.8 and PSV is 10-15
Assessment of endometrium
Endometrial receptivity markers
| Conventional | New |
|---|---|
| Thickness | 3D endometrial volume |
| Patterns | 3D endometrial configuration |
| Peristalsis | 3D endometrial vascularization indices |
| Uterine artery flow |
Basal endometrium is assessed on D2 of the cycle when it appears like a thin bright echogenic line. It grows at 0.5 mm/day in proliferative phase and at 0.1mm/day during the luteal phase. A thickness of > 7mm in preovulatory period is associated with higher pregnancy rates.
Appelbaum’s uterine scoring system (Uterine biophysical profile-UBP)
This is based on certain parameters like endometrial thickness, endometrial layering, endometrial motion and myometrial echogenicity, uterine artery doppler flow, endometrial blood flow within zone 3 and myometrial blood flow ( gray scale). A score of less than 13 was found to be associated with no conception. Endometrial volume as measured by 3D can diagnose adhesions, uterine anomalies and adenomyosis. Most pregnancies occur when volume is 2-13ml.
Endometrial vascular flow indices
They are measured by 3D power histogram analysis. Vascularization Index(VI) flow index (FI) and VFI is a combination of vascularity and flow intensity. Flow indices are lower in stimulated cycles than un-stimulated ones. In IVF cycles high E2 levels lower the flow indices.
Abnormal responses in ovarian stimulation
- Poor response < 2-3 follicles on D7
- Hyper response-Increased number of small and intermediate follicles
- Premature luteinization-Follicle <15mm + Internal echoes+ raised P4
- LUF-34-36 mm, thick walled follicles+ internal echoes even 48h after trigger +thick echogenic endometrium+ no free fluid in POD.
- Endogenous LH surge-Premature rupture of follicles at < 16 mm
- Functional cyst- Cyst with sharp edges, present at baseline scan because of initial high FSH
- Persistent/ retention cyst- Corpus luteum from previous cycle.
For more info, Visit : www.medlineacademics.com