Monitoring of Ovarian stimulation - Part I
Ovulation is induced in anovulatory cycles. This could be for timed intercourse or IUI or for IVF/ ICSi. The aim could be for a mono-follicular response or for multi-follicular growth with controlled ovarian Stimulation (COS)
Monitoring of ovarian stimulation is necessary to optimise the outcome by modifying the dosage of stimulating medications and also to prevent complications like OHSS.
Stages of Monitoring
- Monitoring before stimulation
Transvaginal scan for antral follicular count (AFC) , assessing that the endometrium is satisfactorily downregulated and to rule out any other pathology. Done on day 2 of the menstrual cycle. - Monitoring during stimulation
To determine the response to ovulogens, to titrate the dose of gonadotropins ( step up or step down), to detect premature LH surge, to determine the optimal time for trigger, to detect ovulation, assess risk, diagnose and monitor ovarian hyperstimulation and to determine the time for oocyte retrieval. - Monitoring after stimulation
To establish ovulation, to establish an optimal response to trigger, to identify LUF (luteinized unruptured follicle) or retention/ functional cyst and finally to confirm pregnancy.
Methods of monitoring:
- Biochemical/ Hormonal monitoring
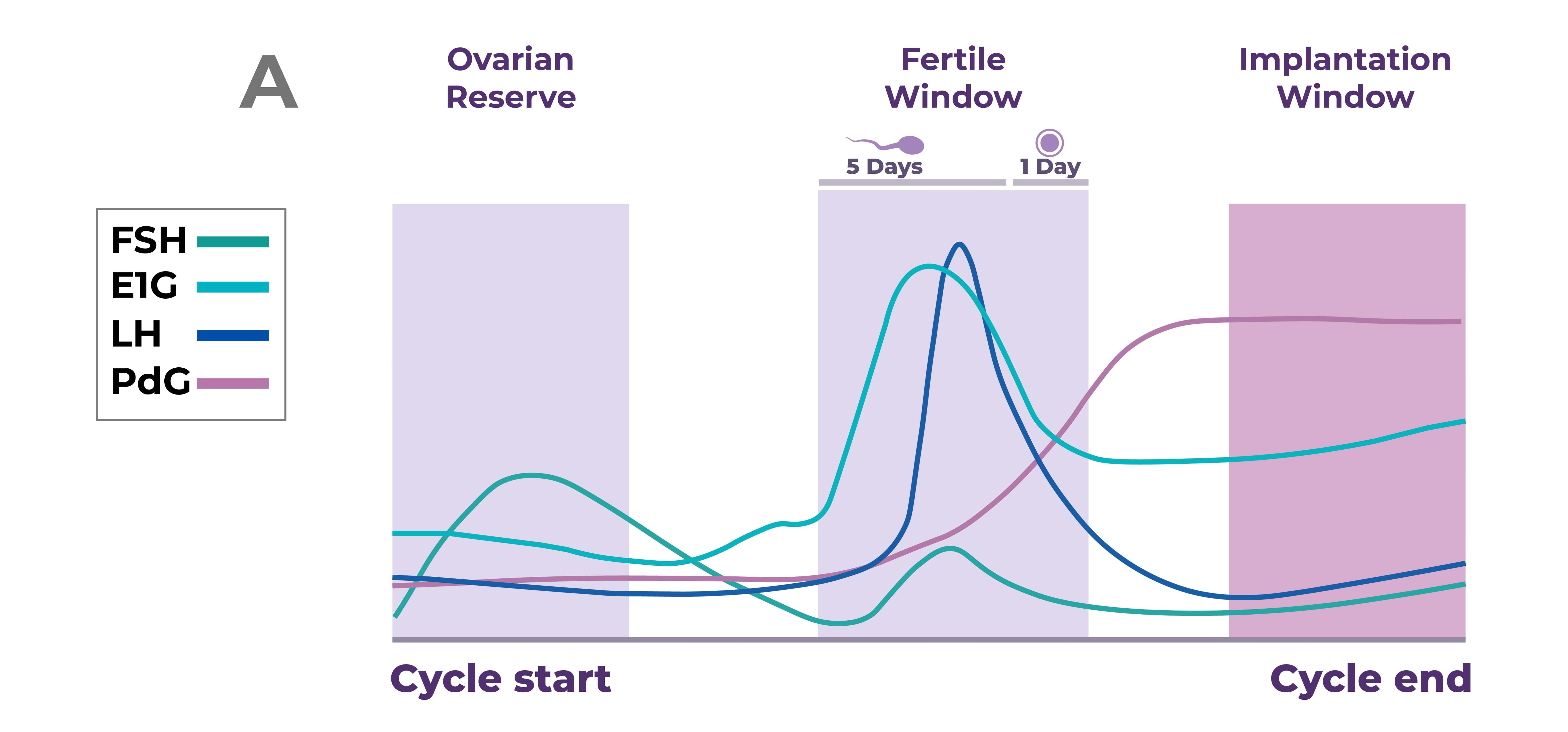
- Hormonal assays of AMH, FSH, LH, Estradiol, Inhibin B, Progesterone
- Home monitoring- Basal Body Temperature (BBT), Cervical mucus testing, salivary ferning assessment, Urinary LH etc.
- Clinical monitoring ( follicular growth & endometrial assessment)
- Transvaginal ultrasound, 2D, 3D and color Doppler
- SOET (Self-operated endovaginal telemonitoring.
Choosing the methods of monitoring stimulation
For advising timed intercourse, BBT, Cervical mucus testing, Salivary ferning, Urinary LH or TVS can be used. TVS is the preferred method of monitoring IUI cycles and for IVF, TVS must be done along with hormone estimation.
The monitoring methos ought to be easy, reliable, cost-effective and patient-friendly.
Home Monitoring
This is by checking the BBT, cervical mucus , salivary ferning assessment and urinary LH kits.
BBT
Progesterone is thermogenic and causes a rise in body temperature, of 0.50 F after ovulation. Progesterone levels are > 3-5ng/ml, 1-5 days after LH surge. Ovulatory cycles have a bi-phasic response. There is a dip in the BBT of 0.4-0.80 F; that is the temperature is 97-980 F on the day of ovulation. Though this is low cost, easy and non-invasive it is a retrospective diagnosis of ovulation and can be affected by patient factors like improper compliance, smoking, alcohol, exercise, anxiety etc.
Cervical Mucus assessment
Preovulatory estrogen rise causes typical changes in the cervical mucus.
The modified Insler score relies on parameters like appearance of OS, mucus quantity, Spinbarkeit. Mucus cellularity and ferning. However, this cannot determine the exact time of ovulation and there exist individual variations in the response of cervical glands to estrogen.
Salivary ferning assessment
During ovulation, the increased estradiol levels causes similar biochemical changes in saliva like in the cervical mucus. Increase salivary NaCl concentration causes crystallization and hence ferning pattern. Commercial kits have 78% specificity and 80% sensitivity to detect salivary ferning.
Electronic resistance evaluation of saliva and vaginal secretions
This is measured by a device called CUE fertility monitor. This can predict the ovulatory window with oral or vaginal probe. Raised LH causes changes in NaCl and other electrolytes in saliva and vaginal secretions. Though it is reusable and can be used at home, it is costly and there have been conflicting jreports about accuracy.
Urinary LH kits
Ovulation occurs 14-26 hours after LH surge . Testing for urinary LH is recommended late afternoon to early evening ( 4-10PM) . A positive result can predict ovulation in the next 24-48 hours with over 90% accuracy. Several factors interfere with the accuracy of LH kits and these include-Endometriosis, PCOS, LUF, hyperthyroidism, renal failure, medications like menotropin, danazol, clomiphene citrate etc. LH surge can be missed in women with irregular cycles and it cannot detect LUF.
{Continued as Monitoring of Ovarian Stimulation- Part II ( Ultrasound Monitoring)}
For more info, Visit : www.medlineacademics.com