Genetic evaluation of infertile men
There are over 200 genetic conditions associated with male in fertility.
Aneuploidies, structural chromosomal abnormalities, autosomal gene mutation, polymorphism, X linked and mitochondrial DNA defects and epigenetic errors are the various ways genes can affect fertility of men. MMAF (Multiple Morphological Abnormalities of the sperm Flagella) is an another entity which includes flagella defects like coiled, bent, irregular, short or absent flagella and also contributes to infertility. Mutations in autosomal genes are known to cause MMAF.
Genetic tests offered to Infertile men:
| Diagnosis | Genetic testing to be done |
|---|---|
| Nonobstructive azoospermia | karyotype and no chromosome microdeletions |
| Obstructive azoospermia | CFTR gene mutation |
| Oligozoospermia | Karyotyping and Y chromosome microdeletions |
| Azoospermia and oligozoospermia with normal karyotype and no Y chromosome microdeletions | Exome analysis |
| Multiple morphological abnormalities of the sperm flagella (MMAF) | Panel for DNAH1, CFAP43, CFAP44, and CFAP69 genes or exome analysis |
| Asthenozoospermia | Exome analysis |
| (CFTR: cystic fibrosis transmembrane conductance regulator) | |
Non-obstructive azoospermia and oligozoospermia
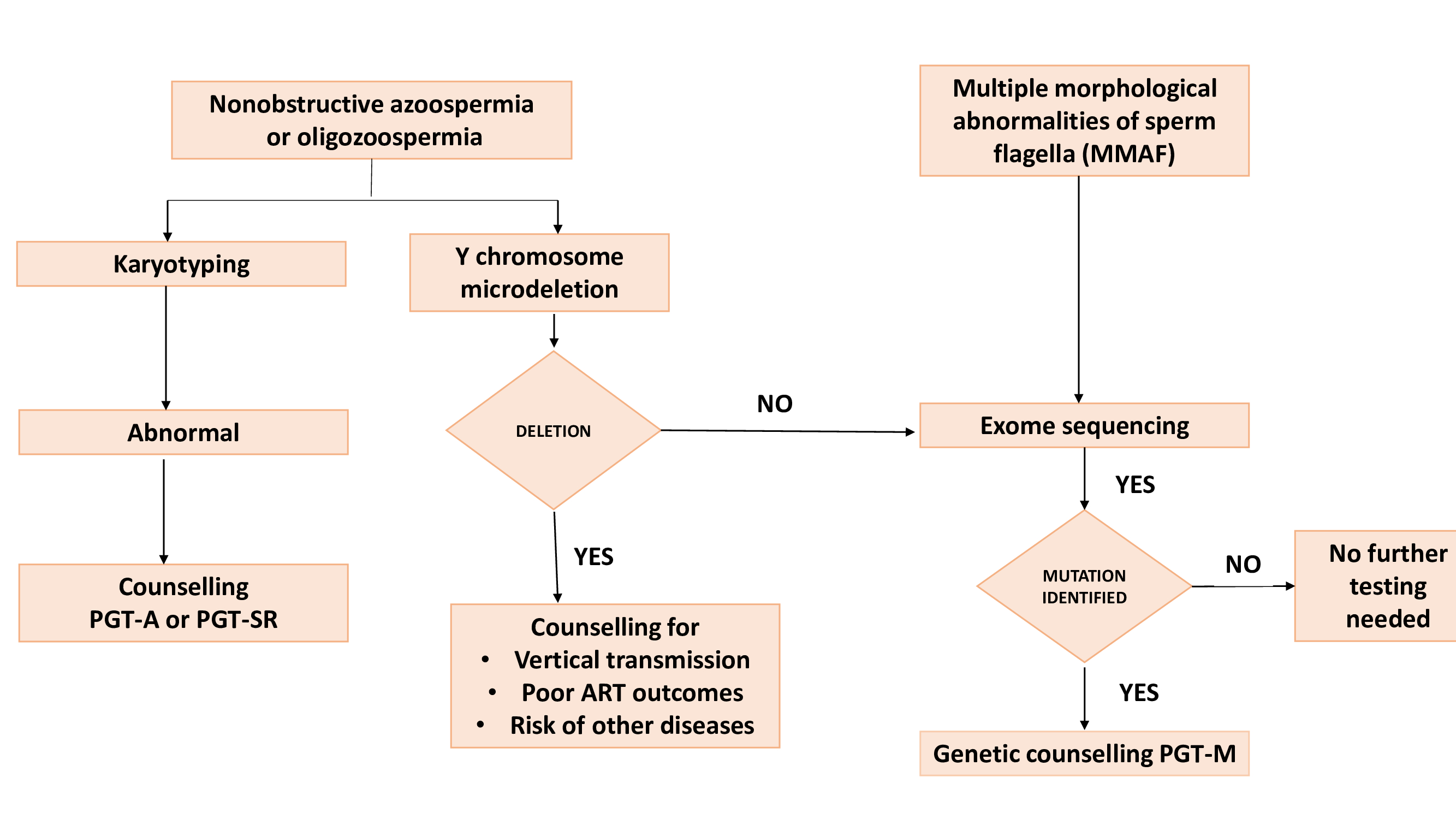
About 10 to 15% of NOA/oligozoospermia will have karyotype abnormalities. Mosaic and non- mosaic Klinefelter syndrome, Dela Chappell syndrome (46 XX with male phenotype), structural abnormalities like Robertsonian translocation, inversions truncated Y, ring Y, isodicentric Y are some of the genetic abnormalities that may be encountered. Polymorphisms of chromosome 1, 9 and 16 may sometimes be normal and should not be considered as pathological. Geneticist consultation is imperative to understand the prognosis and for further course of action. Except in 46 XX phenotypic males, there is a good possibility of getting sperms by testicular sperm aspiration. However, the success rates with ICSI are low. PGT-A or PGT-SR is offered for couple with karyotype abnormalities.
Y chromosome micro deletions cannot be identified on karyotyping but needs PCR testing. ICMR, ASRM and EAA recommend testing for Y chromosome micro deletion in all men with NOA or oligozoospermia. the AZFa, AZFb And AZFc genes are associated with spermatogenesis. The AZFc sub deletion gtr/gtr has a higher incidence in India. Hence we must have Y-chromosome micro deletion testing with appropriate markers for the local population.
Hormones &/or antioxidants, lifestyle changes, varicose vein surgery which are often offered to oligospermia men do not help those with why micro-deletions, AZFa and AZFb as there will be no sperms in the testes. TESE is avoided in them. Men with AZFc microdeletions can have hypospermatogenesis and TESA can be tried. However, embryos from the men with Y-micro deletions are poor in quality and have impact blastocyst rate and report reduced success with ART. These men must be counselled about vertical transmission and that all male off-springs will inherit the same microdeletion.
Men with y chromosome microdeletion have a predisposition to testicular germ cell tumour, mild to severe psychiatric disorders with increasing age. Loss of Y-chromosome is also associated with increased risk of heart failure, age related macular degeneration, colorectal and prostate cancer.
Testing for other chromosomal abnormalities is currently not a routine because it is still under research.
Algorithm for genetic testing in men with NOA, Oligospermia and MMAF
Obstructive azoospermia
There are 5 phenotypes of absent vas deferens. They are:
- CBAVD (Congenital bilateral absence of vas deference)
- CBAVD + URA (unilateral renal abnormality)
- CUAVD (Congenital unilateral absence of vas deferens)
- CUAVD +URA
- CBAVD/CUAVD + EDO (Ejaculatory duct obstruction)
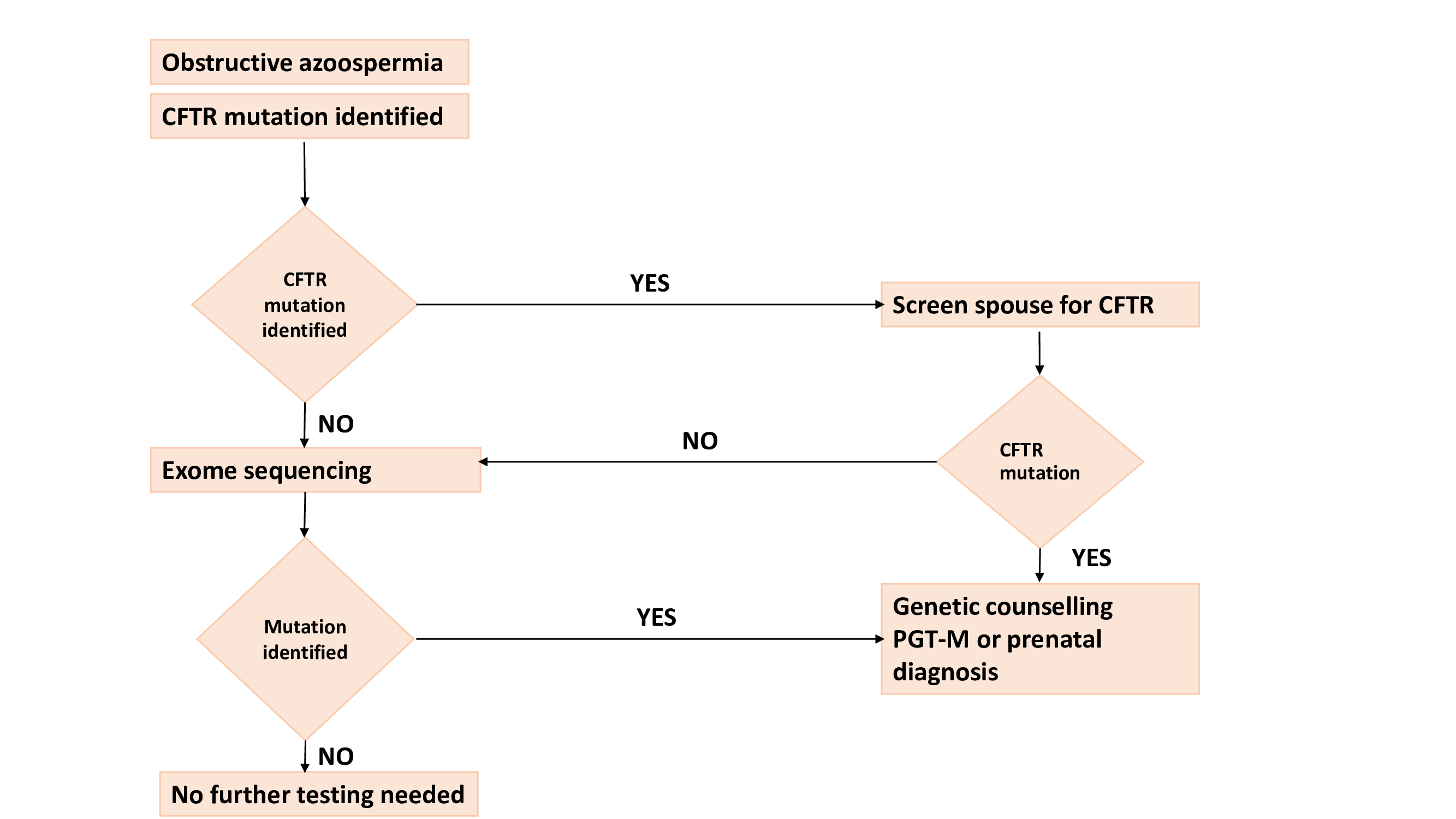
The CFTR ( Cystic Fibrosis Transmembrane Conductance Regulator) gene is seen in 60 to 70% of men with CBAVD, whereas 30 to 40% cases may have another genetic defect. There are 2 types of CFTR mutations- severe and mild. Men with 2 severe mutations have cystic fibrosis and about 90% of cases have one mild and one severe mutation, while 10% of cases have 2 mild mutations. CBAVD without CFTR mutation can exist with but some pathogenic mutations like ADGRG2, PANK2, SLNN1B, CA12. However, their functional significance and pathogenesis is still under investigation and therefore they are not used in routine practice.
TESA-ICSI can be offered for men with CBAVD as there is active spermatogenesis and good quality sperms can be retrieved.
Algorithm for genetic testing in men with obstructive azoospermia
MMAF (Multiple morphological abnormalities of flagella).
In men with this problem, semen samples shows total asthenozoospermia with varied sperm flagellar anomalies. However the latest WHO manual does not provide any classification for MMAF and hence it is not a part of routine reporting. Such patients are very likely to have genetic defects. Mutations have been reported in DNAH1,CFAP43, CFAP44 and CFAP69 genes.
However, genetic cause accounts for only 30% of MMAF and cause in others is not known. Whole Exome Sequencing is needed for detection of any such genetic abnormalities but currently it is not possible in a clinical laboratory and needs further research.
Men with MMAF cannot improve with medical therapy and hence ICSI is the only option. There are limited reports of outcome with fertilization rates reported as 40-75% and clinical pregnancy rate as 50%. In some men with MMAF with mutations in autosomal genes, the functions of organs where ciliary activity is needed-like lungs/ brains- may also be affected. There is no information on health outcomes in men with MMAF. PGT-M is a must for men with MMAF who have undergone ICSI. But utility of gene mutation testing for MMAF is still in infancy
To conclude, it is imperative to do appropriate genetic testing in cases of non obstructive and azoospermia and severe oligospermia. Geneticist consultation and counselling is very important for this couple and they will most often need TESE/ ICSI and then PGT.
