Fertility Preservation
What is Fertility Preservation?
It can be defined as a means of preserving an individual’s ability to reproduce at will or at a chosen time. In this era of advancement in medical care and facilities, fertility preservation has given a new dimension to assisted reproductive technology (ART) services. This method helps patients to have a biological child whenever they want in the future.
Who Is It For?
Fertility preservation is a great way to protecting and saving an individual’s gamete or embryo or reproductive tissues. This can be utilized by both male and female, and people of LGBTQ+ community.
Why Is It Done?
Some of the reasons for undergoing fertility preservation are as follows.
- Advanced age
- Women: Women with advancing maternal age have difficulty conceiving due to age related changes in their reproductive function. Fertility of women above 32 years starts declining and this decline accelerates after the age of 37 years. Personal reasons for women wanting to delay childbirth are waiting for the right partner/spouse or waiting until they are professionally established.
- Men: Advancing paternal age > 40 years is associated with declining sperm quality, increased risk of pregnancy complications, birth defects, childhood cancers, autism, and some psychiatric disorders.
- Oncological reasons (Cancer)
In today’s world, there is a marked increase in the incidence of cancer worldwide in both the genders and in all age groups. With the advancement in diagnosis and treatment of cancer, there is also growing pool of cancer survivors who wish to have a family of their own in the future.- Women: Cancer therapy in women leads to premature ovarian insufficiency (POI) because of the effect of chemotherapy and radiotherapy on the ovary.
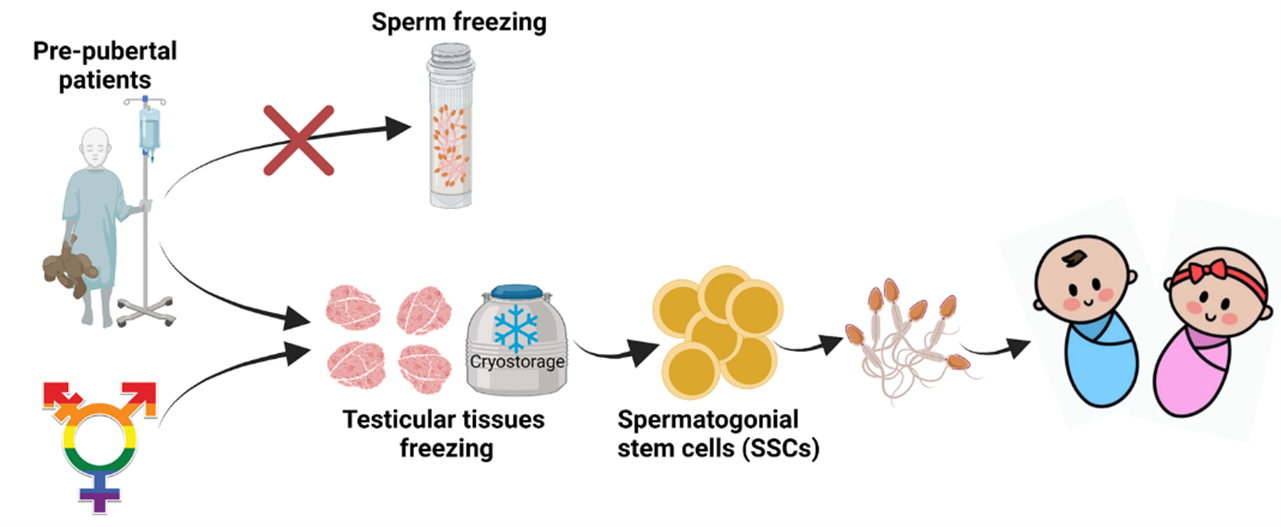
- Men: Cancer incidence and survival in prepubertal, pubertal and post pubertal men have increased substantially and men of all group plan for preserving their ability to father a child before starting gonadotoxic treatments.
- Benign conditions
Women: Reproductive health conditions such as endometriosis, uterine fibroid, etc.
Men: spinal cord injuries, HIV, men planning to go for vasectomy, etc. - Autoimmune disorders
Women:
Some of the autoimmune conditions which affects the fertility potential are as follows.- SLE
- Behcet’s syndrome
- Sjogren’s syndrome
- Steroid resistant glomerulonephritis
- Inflammatory bowel disease
- Scleroderma
Men: Treatment of some of the autoimmune diseases such as SLE, Crohn’s disease, multiple sclerosis require hematopoietic stem cell transplantation which in turn requires chemotherapy and radiotherapy which also damages the spermatogonia. - Transgender care
People undergoing gender affirming treatments are given an option for fertility preservation before their treatment since the gender affirming medicines and surgeries affect their fertility. - Other reasons
Posthumous sperm retrieval, which refers to retrieval of gametes and reproductive tissue after a person’s death or after they have become incapacitated, and their death is imminent. It refers to a situation where the person will be deceased at the time their gametes are used, and any resulting child is born.
How Is A Person’s Fertility Affected?
1. Cancer

A. Chemotherapy
Cancer treatments include chemotherapy and radiotherapy.
Chemotherapeutic agents cause single and double strand DNA breaks in the gonadal cells.
Among the chemotherapeutic agents alkylating agents such as cyclophosphamide, chlorambucil, busulfan and mechlorethamine have maximum negative impact.
Mechanism of cellular damage in women
- DNA damage in ovarian cells
- Ovarian cortical fibrosis
- Ovarian blood vessel damage
- Premature menopause
- Ovarian insufficiency
- Poor reproductive outcomes
Mechanism of cellular damage in men
Cytotoxic therapy causes,
- Damage to spermatogonial stem cells.
- Damage to differentiating germ cells.
- Damage to Sertoli cells.
- Damage to leydic cells.
It has also been observed that the adverse effects of the treatment on fertility may be reversible in men.
B. Radiotherapy
Radiotherapy involves irradiation at different doses to kill the cancer cells. However, these radiations are damaging to highly mitotically active gonadal cells as well.
Ovary: Irradiation dose as low as 2 Gy can destroy 50% of the primordial follicles in the ovary. It has also been observed childhood and prepubertal irradiation caused many women to suffer from premature ovarian failure.
Testis: Irradiation affects the spermatogonial stem cells and thereby results in fertility problems.
C. Cancer Surgeries
Debulking surgeries is one of the treatments in cancer patients which causes both direct damage and indirect damage to spermatogenesis. Procedures like orchidectomy causes direct damage, however damage to sympathetic and parasympathetic nervous system during surgery causes ejaculatory and erectile dysfunction in men.
2. Gender Reaffirmation Treatments
Many transgender people opt for gender reaffirmation treatments. Sex affirmation treatment in men and women involve cross sex hormone therapy and surgery to remove ovary/ testis which will have a deleterious effect on the fertility of these individuals.
3. Other Conditions
Women
Genetic disorders: In women, some of the genetic condition which predispose to premature ovarian insufficiency are as follows.
- Turner syndrome
- Fragile X syndrome
- Galactosemia
Surgeries: Endometriosis treatment involve corrective surgeries which can cause local inflammation which increases the follicular burnout and affects fertility by altering the ovarian reserve.
Men
HIV: It has a direct impact on fertility. It is associated with abnormal seminal parameters. It also depends on the age, duration, and presence of other STDs.
Vasectomy: It is a permanent method of contraception. Many men who have undergone request a reversal of the procedure due to a change in their life circumstances. Option of fertility preservation before vasectomy may be considered.
Techniques Of Male Fertility Preservation
1. Sperm cryopreservation

It is a most common technique utilized for fertility preservation. Although the exact length of time that cryopreserved sperm remains viable is unknown, there are reports of successful parenting using sperms which has been stored for up to 28 years. In patients with ejaculatory dysfunction, TESA and Micro- TESE can be done. The main disadvantage of this method is that it cannot be to of use in prepubertal boys.
2. Testicular tissue cryopreservation
It is an option for prepubertal patients. The main disadvantage of this method is that of decreased cell survival with a post thaw viability of around 60%. Additionally, there is also a concern regarding reseeding the cancer when the cryopreserved tissue is reintroduced into the host.
3. Other methods
Gonadal shielding is done to prevent damage to the spermatogenic stems cells in the testes due to radiation. It is done by covering the testicular region with a lead shield. Gonadal suppression with the GnRH agonists and antagonists may help in recovering the spermatogenesis after exposure to the toxic therapy.
Techniques Of Female Fertility Preservation
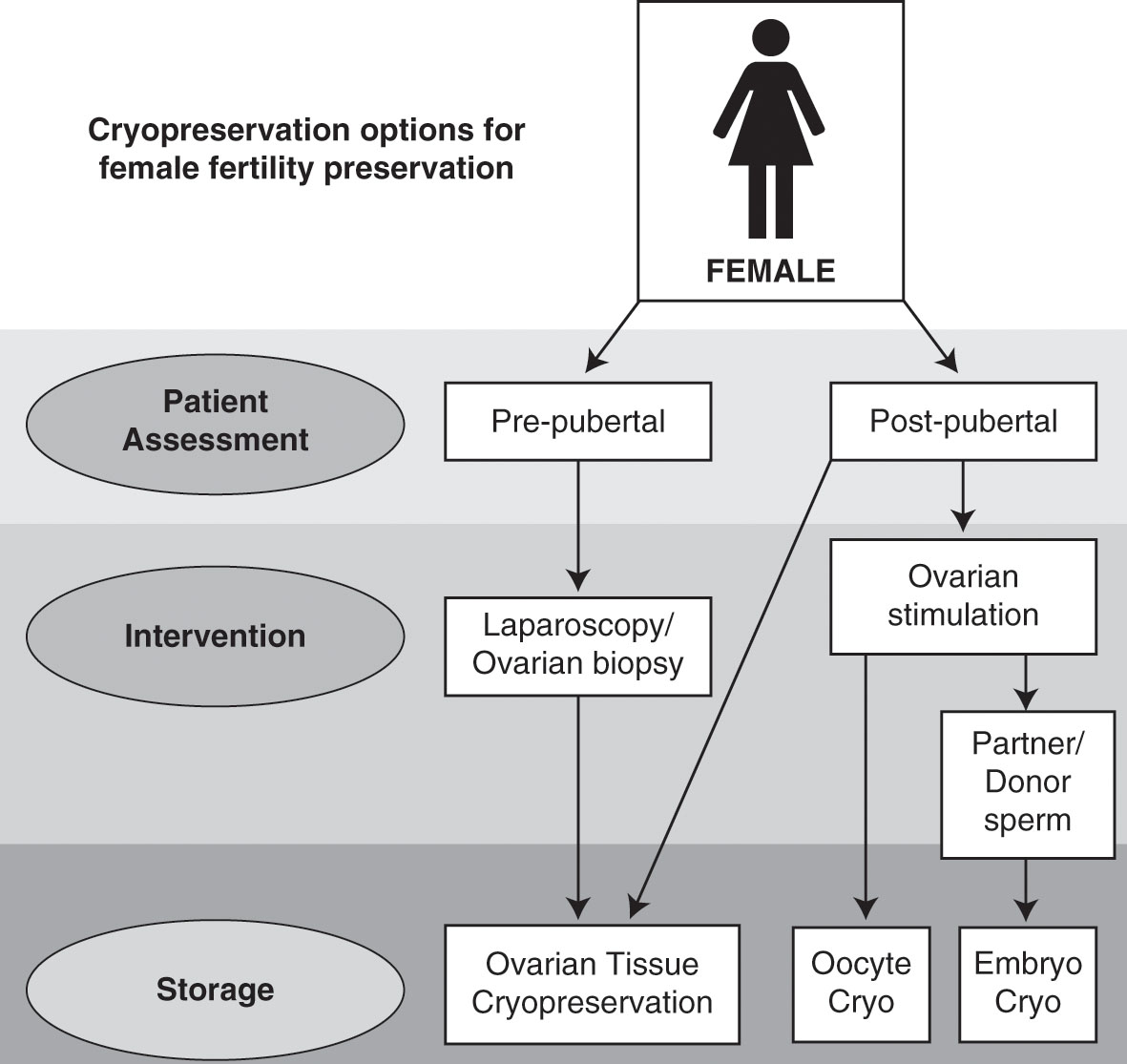
The options of fertility preservation should be discussed with the patients before starting any treatment. The choice or optimal method of preservation depends on age, time available, presence or absence of a partner and the nature of the condition. The following are the options available.
1. Embryo cryopreservation

In women of post pubertal age group is ideal for this method, where before the patient is treated for ovarian stimulation for 2 weeks followed by egg retrieval and cryopreservation. The main advantage of this method is that embryo survival, implantation and pregnancy rates are relatively higher when compared to oocytes. The main disadvantage is that it cannot be used in women of prepubertal age group.
2. Oocyte cryopreservation
This is the ideal method for women without partners. The main draw back is that oocytes are more vulnerable to damage by the vitrification and thawing process than embryos.
3. Ovarian tissue cryopreservation
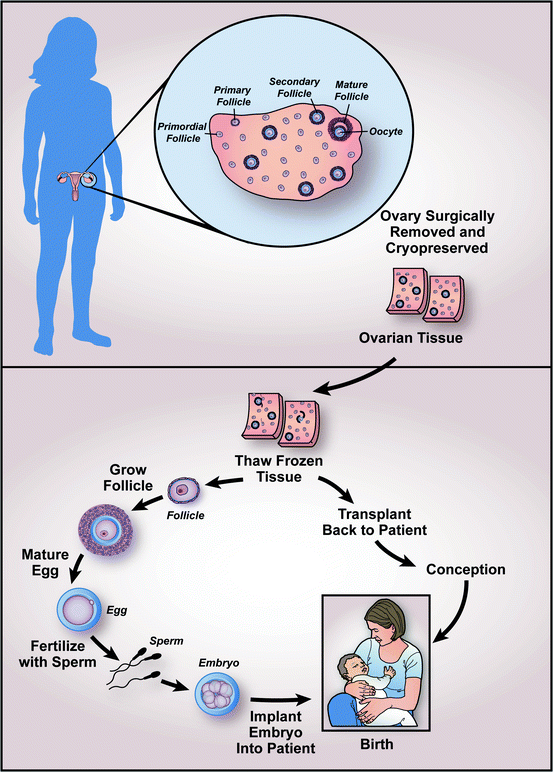
In this method, the ovary can be cryopreserved as a whole or just the cortical tissue which contains the follicles. Usually, slow freezing is used than vitrification. When the patient likes to start family, the cryopreserved tissue can either be transplanted back into the patient or in-vitro maturation is performed on the follicles obtained from the tissue. When transplanted back into the patient’s body, it takes 4-6 months for the tissue to become functional and continues its function for approximately 5 years. As per ESHRE guidelines, ovarian tissue cryopreservation can be offered to
- Patients undergoing gonadotoxic treatment where oocyte or embryo cryopreservation is not feasible.
- Patients with genetic or chromosomal conditions with POI
- It should not be offered to women with low ovarian reserve or advanced age.
4. Transposition of Ovaries (Oophoropexy)

In this method, ovaries are moved out of the field of pelvic irradiation to prevent damage. It is offered to women undergoing radiation therapy without chemotherapy. However, it is not for women with low ovarian reserve or at risk of ovarian metastasis.
5. Hormonal suppression
Cancer treatment kills mainly fast dividing cells of the body which also includes the germ cells of the ovary. GnRH agonists treatment reduces the ovarian activity by blocking the hypothalamo-pituitary-gonadal axis and reduces the toxic effects of cancer treatment. This method can also be used in premenopausal women with autoimmune disorders receiving gonadotoxic drugs for treatment.
Conclusion
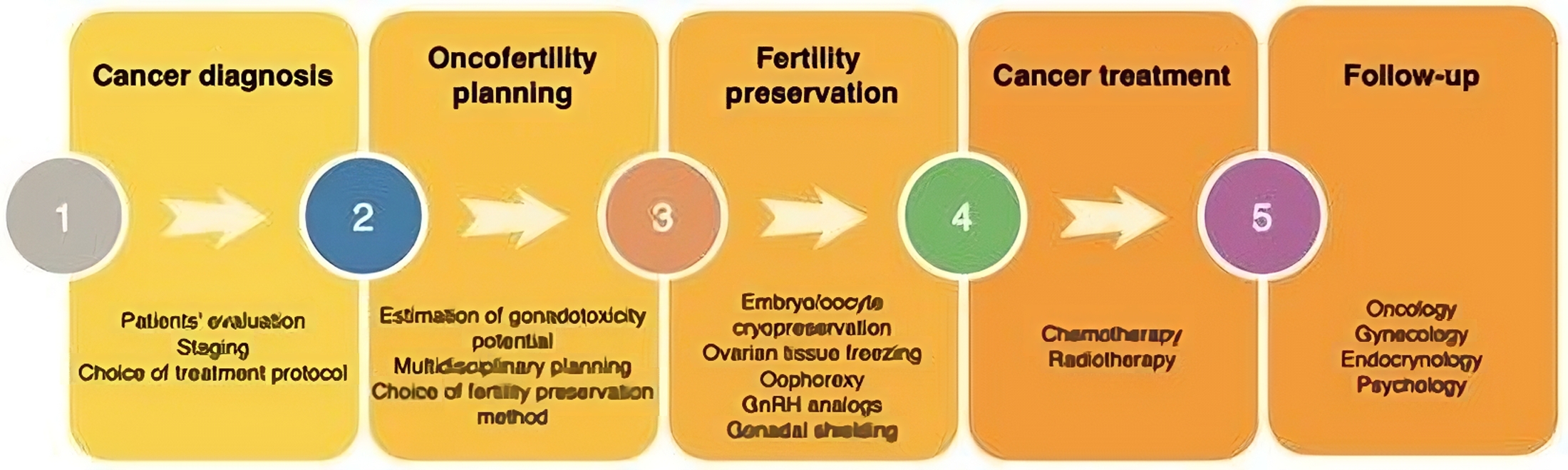
Fertility preservation requires a multidisciplinary approach involving oncologists, onco-surgeons, infertility specialists and embryologists. Every patient undergoing cancer treatment should be informed about all the options available for fertility preservation and should be done prior to initiating cancer treatment. Prepubertal men and women have testicular tissue cryopreservation and ovarian tissue cryopreservation as a method of preserving their fertility. In post pubertal men sperm cryopreservation can be done and in post pubertal women oocyte/embryo cryopreservation are well established. Other strategies in men and women are in experimental stages. Apart from all the advancements, when it comes to posthumous reproduction, we should also consider the psychological, ethical, and legal issues involved in it.
If you are looking to advance your career and expand your knowledge in the field of infertility, join our Fellowship in Reproductive Medicine Program at Medline Academics stands. We aim to cultivate a team of professionals who are equipped with cutting-edge knowledge and a deep understanding of infertility. The fellowship offers unique and comprehensive platform for aspiring healthcare professionals who are passionate to know more on all areas of infertility including the transformative field of fertility preservation.
