Uterine factors in infertility - Myomas
Impact of myomas on fertility
Myomas interfere with normal fertility in many ways. The increase the distance for sperm travel, can encroach on the tubal ostia, distort the uterine cavity, interfere with rhythmic uterine contraction, impair implantation, cause abnormal endometrial maturation, cause vascular changes to uterus and cause alteration of oxytocinase activity.
Pathogenesis how myomas interfere with fertility.
Intramural myomas alter the architecture of the myometrium, cause increased intracellular calcium, and cause myometrial irritability and hyperactivity that disrupts the rhythmic contraction of junctional zone. Sub-endometrial myoma causes endometrial erosion, impair local pro-implantation factors creating a hostile environment and affect the blood supply also.
The impact of non-cavitary myomas on fertility is controversial.
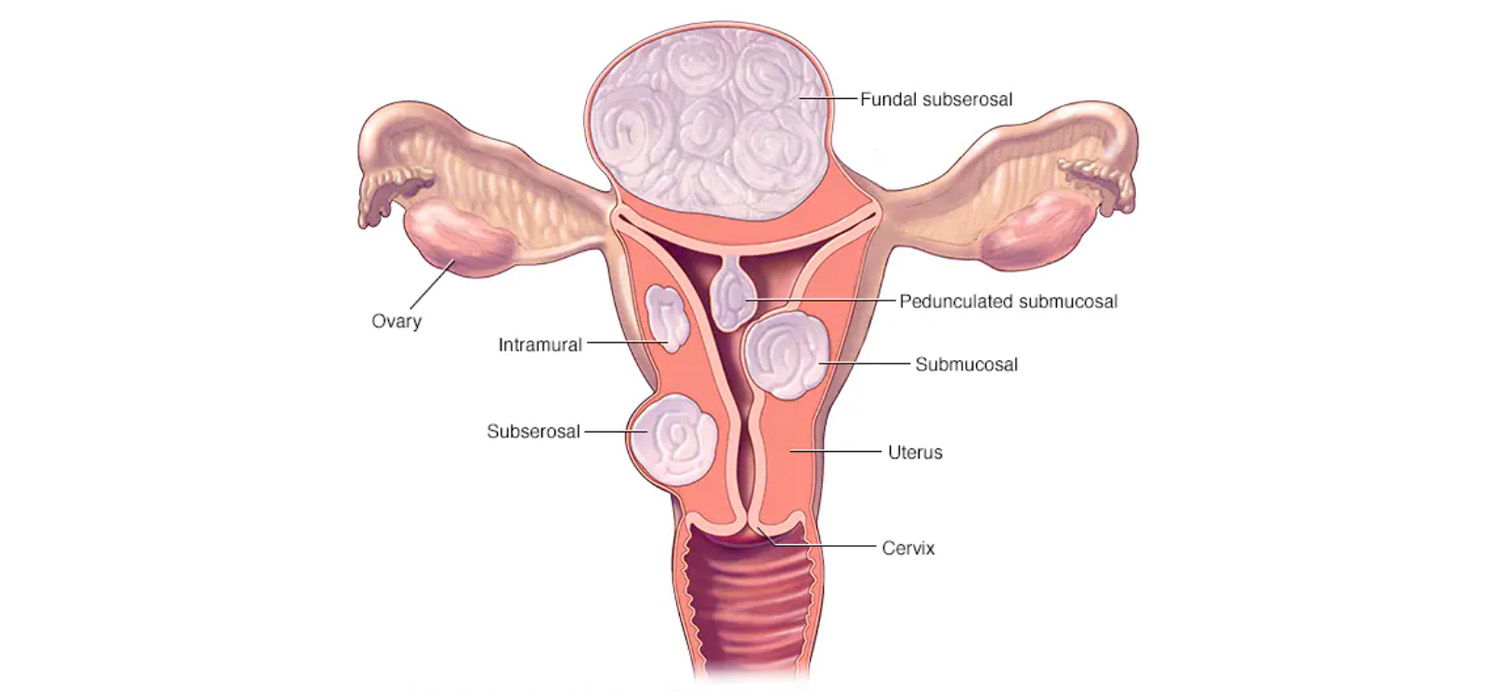
Classification of myoma (FIGO)
0- Pedunculated intracavitary
1- <50% intramural
2- >50% intramural
3- Contacts endometrium
4- Intramural
5- Subserous, >50% intramural
6- Subserous, <50% intramural
7- Subserous pedunculated
8- Others-Cervical, parasitic etc.,
Myomectomy- Indications and controversies:
Myoma may be an incidental finding in many infertile women and only a fraction might benefit from surgery. Recent meta- analysis has shown that leiomyoma without cavitary involvement may also reduce the success rate of ART.
In general, myomectomy is indicated in:
- Recurrent implantation failure.
- Intramural myoma of over 5 cms
- Intramural myoma with submucous extension
- Women with recurrent implantation failure.
Management of submucous myomas
Hysteroscopic removal is indicated for all infertile women with submucous myomas. Abdominal approach is indicated when there are more than three sub-mucous myomas, when hysteroscopic removal can damage a large portion of the endometrium and category 3-7 of the above classification. STEP-W. (Size, topography, Extension, Penetration and Wall) algorithm may be used to plan and prognosticate surgery in submucous myomas. A score of 0-4 indicates less complications and a hysteroscopic method can be employed. Scores of 5,6 suggest pre=treatment GnRH and 2 step hysteroscopic myomectomy. For a score of 7-9, alternate techniques can be considered. Pre-op evaluation included proper history and examination, imaging studies-USG/SSG/MRI/ Hysteroscopy- as indicated, having the right idea about the number and location of the fibroids. Informed consent about the proposed surgery and outcomes, correction of anemia, bowel preparation and considering GnRH pre-treatment are the pre-operative requirements.
Fertility outcomes after myomectomy
Systemic reviews have indicated that myomas reduce fertility and removal of myomas enhances conception. Patients are advised to wait for 2-3 months after myomectomy before trying to conceive. They can attempt for a vaginal delivery too. There have so far been no reported cases of uterine rupture.
Cervical myomas:
Cervical myomas constitute 5% of all the myomas. They must be removed if they restrict entry into the uterine cavity for ART procedures.
Medical management of myomas
This may be indicated when there are multiple small myomas when surgery is more traumatizing. Ulipristal acetate (UPA) in doses of 5-10 mgs per day reduces the size of myoma, volume of the uterus, reduces pelvic pain and bleeding. For large myomas, patients may take two courses of three-month cycle of 5-10 mgs of UPA. Patients can attempt pregnancy after the second bleed, following cessation of therapy.
For more info, Visit : www.medlineacademics.com