Female Genital Tuberculosis and Infertility
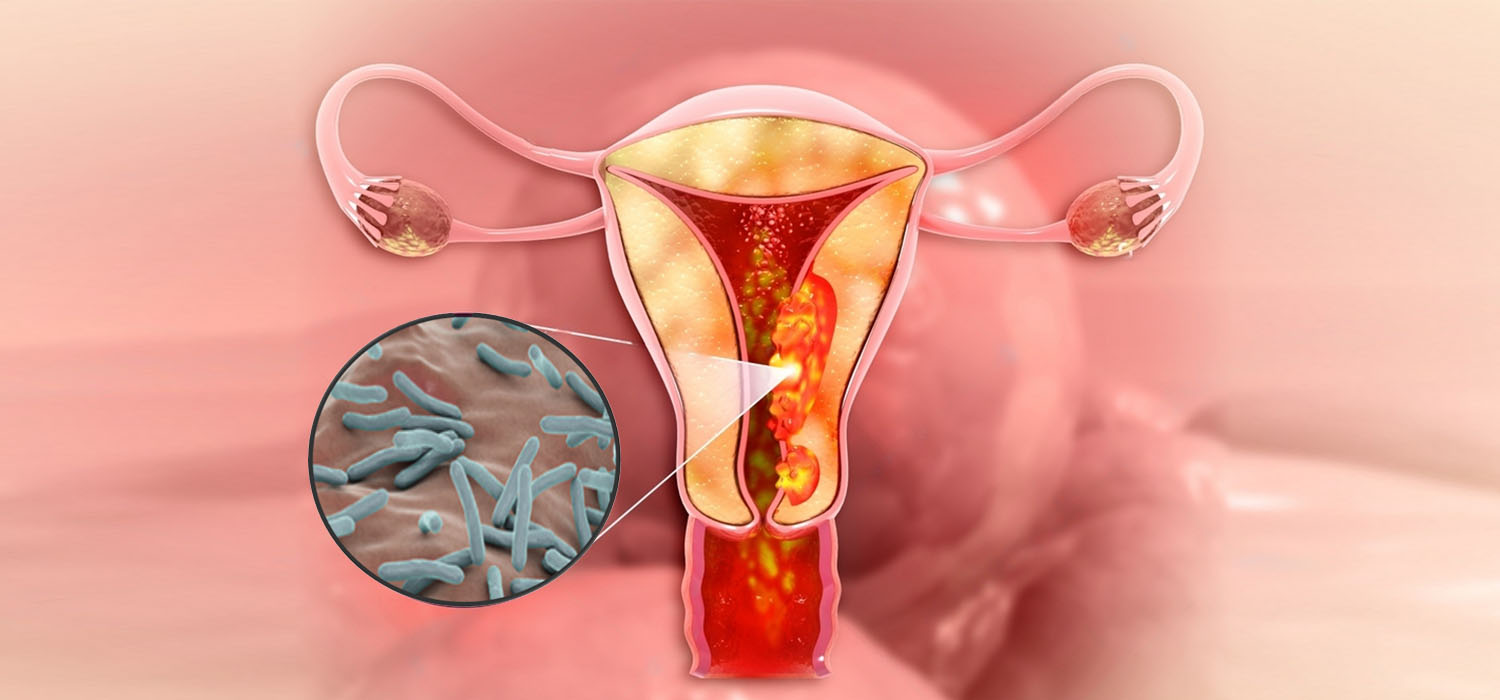
In developing countries, morbidity and mortality because of tuberculosis is high. Mycobacterium tuberculosis primarily affects the lungs; however, genital tuberculosis is seen in a substantial number of men and women. Genital TB in its initial stages is difficult to diagnose because of its asymptomatic and deceptive nature. At times, Infertility could be the only presenting symptom.
There is a significant effect of tuberculosis on women in reproductive age group. Female genital TB (FGTB) is a chronic condition that causes irreversible damage to the genital organs leading to various problems. It is estimated that FGTB accounts for 5% of all pelvic infections in females and is present in 10% of all pulmonary TB cases. It is more commonly seen in developing countries, especially in people with HIV, immune compromised states, and malnutrition. Poverty and poor healthcare facilities are added dangers.
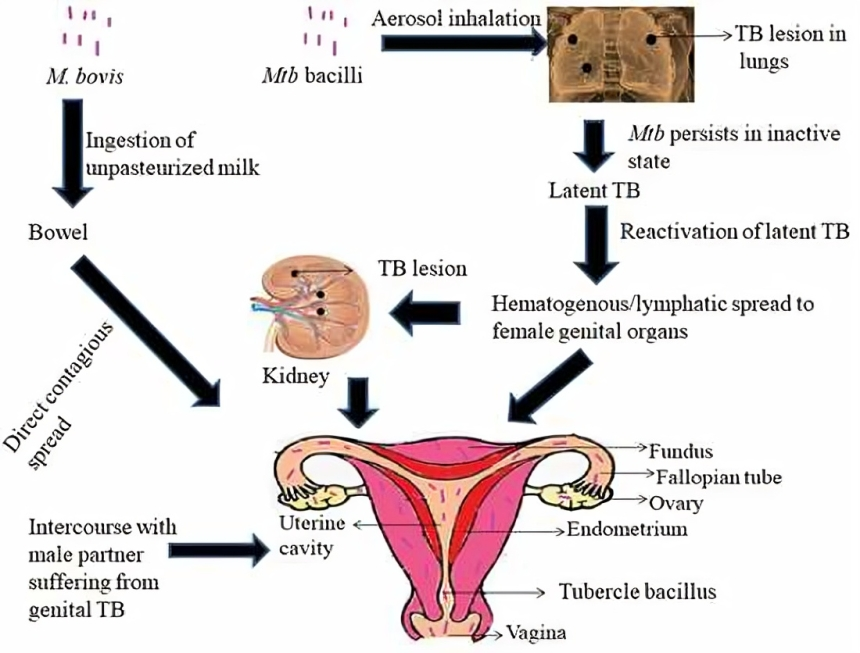
Mode of spread
FGTB is a secondary infection due to pulmonary TB. The mode of spread is by the following
- Hematogenous route
- Lymphatic route
- Direct spread from abdominopelvic TB, peritoneum, and abdominal lymph nodes.
- Direct contact with a male partner having genitourinary TB.
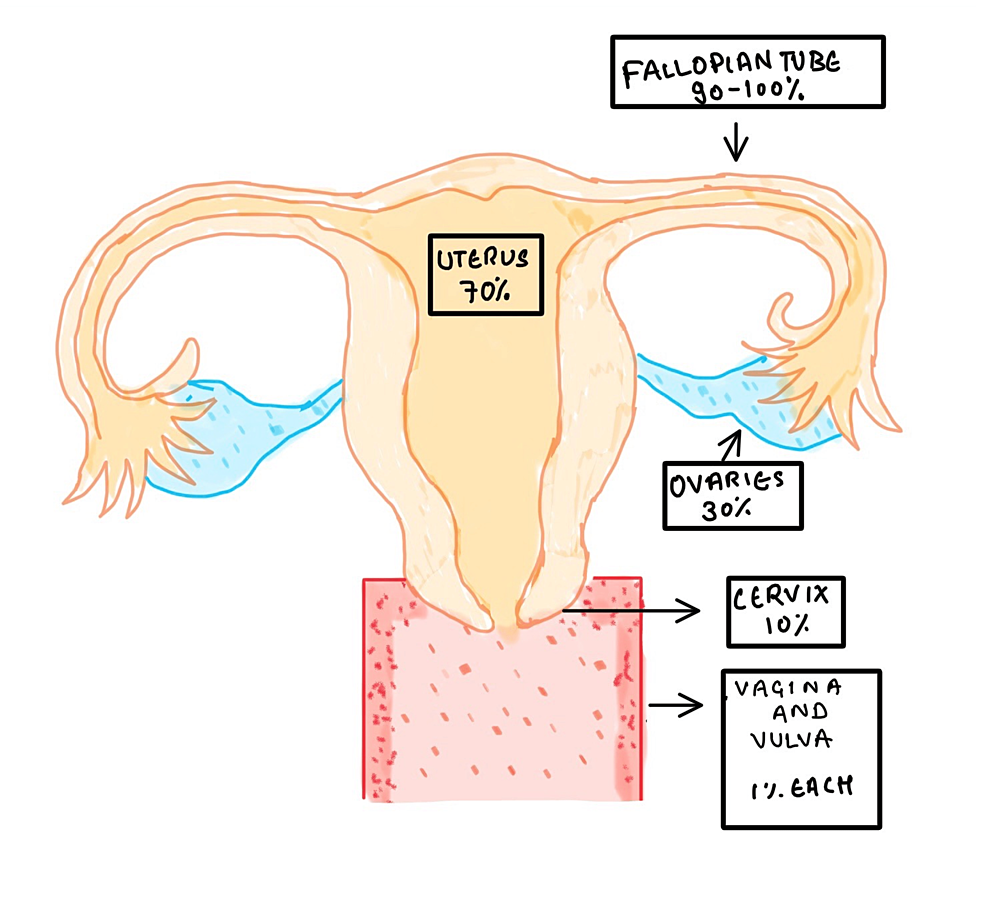
Parts of the female reproductive system affected
The following are the parts affected (presented in the descending order of involvement and their clinical features)
- Fallopian tubes (seen in 90-100% of cases)
- Uterus (70% of cases)
- Ovaries (30% of cases)
- Cervix (10% of cases)
- Vagina (1% of cases)
Main risk factors for FGTB
- Chronic pelvic inflammatory disease resistant to regular antibiotic treatment
- Unknown infertility
- Abnormal Chronic vaginal discharge
- Past/ present history of pulmonary TB
- History of exposure to people with TB
- Immunocompromised state such as HIV
Symptoms
FGTB is underestimated because the majority of the cases are asymptomatic and it is primarily diagnosed only when patients are evaluated for Infertility. Some patients show vague symptoms such as follows
- Irregular menstrual cycle such as oligomenorrhea, amenorrhea, menorrhagia, dysmenorrhea
- Pelvic pain
- Vaginal discharge
- Repeated tubal pregnancy
- Repeated abortions/miscarriages
Clinical findings/ signs
- Adnexal mass- tender fornices
- Frozen pelvis
- Fallopian tubes- Tubal congestion, salpingitis, tubercles, hydrosalpinx, pyosalpinx, tubo-ovarian mass
- Uterus - Asherman’s syndrome, ulceration
- Ovaries- tubo-ovarian mass
- Cervix- Cervical nodules/erosion/hypertrophy
- Vagina -Vaginal/vulval non-healing ulcer
How it causes infertility
Nearly all patients with FGTB have affected fallopian tubes and more than 50% have endometrial involvement.
Fallopian Tubes: FGTB of tubes causes salpingo- peritonitis which leads to adhesions, tuboovarian mass, and hydrosalpinx → which eventually leads to loss of tubal function → which forms the base of infertility by affecting fertilization and embryonic implantation.
Ovary: FGTB causes defective ovulation, chronic anovulation, oocyte defect, poor quality of embryos, and lower progesterone secretion which ultimately affects fertility
Uterus: affects endometrial receptivity and causes atrophy and synechiae formation.
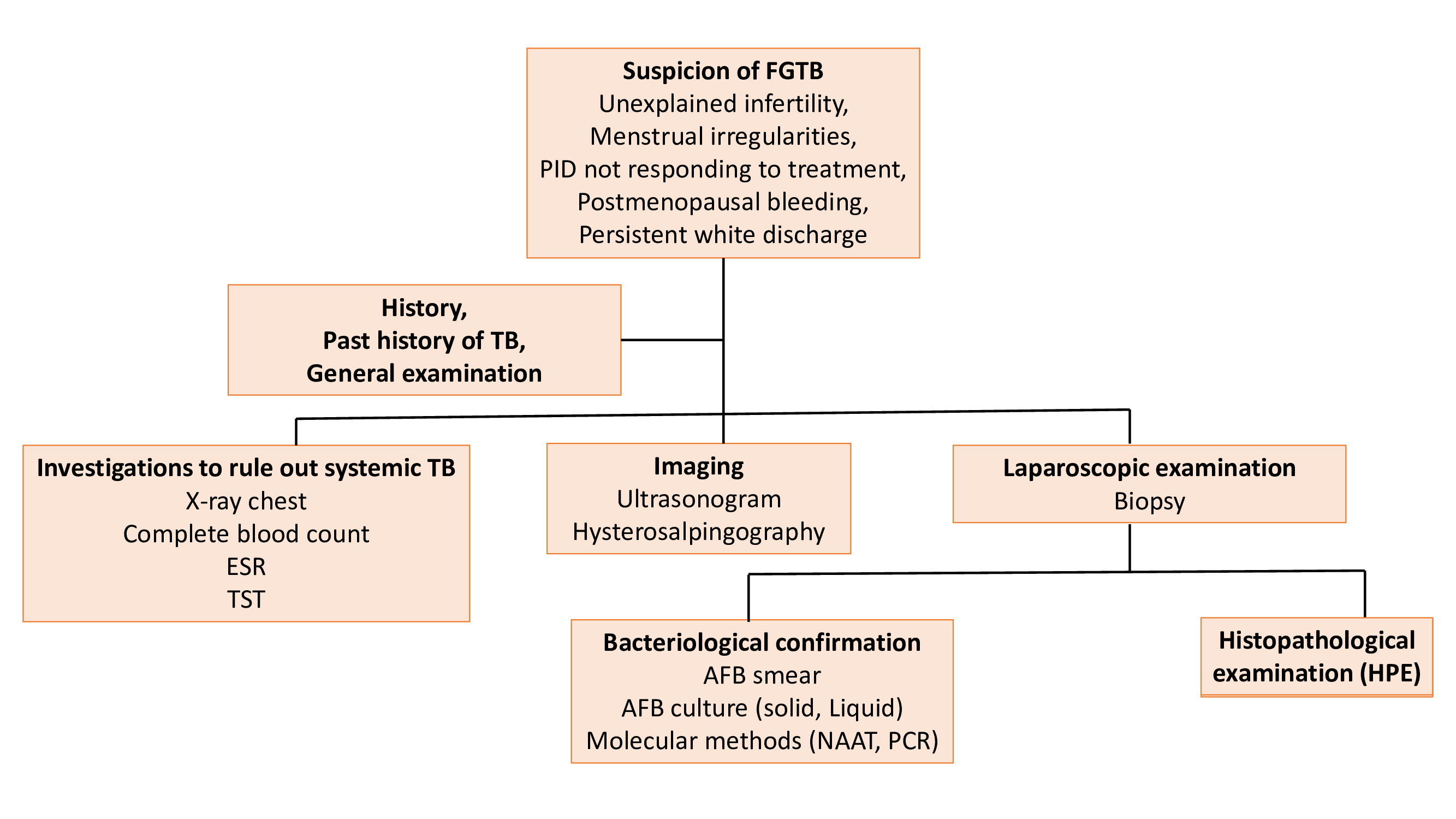
Diagnosis
Due to the paucibacillary nature of the FGTB, easy diagnosis of Mycobacterium Tuberculosis is not possible. Diagnosis should include the following
- Exhaustive history taking including family history of tuberculosis
- Thorough physical and Gynecological examination
- Appropriate use of tests such as
- HSG - is recognized as the most accurate method for detecting FGTB and the gold standard method for determining tubal infertility.
- Tubal findings: beaded tube, leopard skin tube/ cobblestone tube/ golf club tube/ pipestem tube/ cotton wool plug
- Uterine findings: collar-stud abscess/ T-shaped uterus/ pseudo unicornuate uterus/ Netter syndrome
- USG: hydrosalpinx/pyosalpinx/ tuboovarian mass
- CT and MRI: abdominal or pelvic mass
- Laparoscopy With Hysteroscopy: tubercles on the surface, adhesions, tubo-ovarian mass/ hydrosalpinx
- Histopathological Examination: granulomatous caseous lesions with giant epitheloid cells
- Bacteriological Evaluation:
- AFB Staining
- Culture
- Molecular methods:
- NAAT (nucleic acid amplification tests)
- PCR: it has the benefit of high sensitivity and specificity, and rapid turnaround time. However, there is a disadvantage of a high false positivity rate.
- SEROLOGY
- GeneXpert MTB/RIF: Here there is simultaneous detection of M. tuberculosis and resistance to rifampicin. Results can be obtained in less than two hours. It has high specificity and less sensitivity
- HSG - is recognized as the most accurate method for detecting FGTB and the gold standard method for determining tubal infertility.
Differential diagnosis
In the management of infertility and other conditions, it is very important to identify other conditions that show clinical similarities to FGTB. It is very important to rule out other conditions such as cervical/ ovarian cancer. The following table shows some of the common differential diagnosis.
| Site of involvement | Differential diagnosis |
|---|---|
| Tuberculous salpingitis | Pelvic inflammatory disease Ectopic pregnancy Ovarian cyst Carcinoma of the colon Diverticulitis |
| Endometrial tuberculosis | Dysfunctional uterine bleeding Endometrial carcinoma |
| Ovarian tuberculosis | Ovarian malignancy |
| Cervial tuberculosis | Carcinoma of the cervix |
| Vulval tuberculosis | Elephantiasis vulva |
Treatment of FGTB
Medical Treatment: Anti-tubercular treatment (ATT) is given for a specific period. Drugs used are Rifampicin, isoniazid, pyrazinamide, and ethambutol.
Surgical Treatment: Fertility enhancement surgeries such as Surgery for hydrosalpinx, pyosalpinx, tubo-ovarian mass/ abscess, pelvic adhesions, Asherman’s syndrome, etc. can help patients with infertility.
Assisted Reproduction:
Since the long-term effect of FGTB is irreversible, fertility is not reversed even after ATT treatment. IVF treatment gives better pregnancy outcomes if the diagnosis is done early. Poor response to IVF treatment could be due to poor oocyte quality/poor ovarian reserve/ poor endometrial receptivity. In such cases, third-party reproduction is beneficial through oocyte donor or surrogacy.
Conclusion
FGTB significantly contributes to infertility, especially in underdeveloped and developing nations. It greatly impacts female fertility and stands as the primary cause of tubal factor infertility. The organism Mycobacterium tuberculosis is known to survive in our bodies and cause active disease even after decades, whenever the host immunity is decreased. Because of the paucibacillary nature of the organism, diagnosing the disease in its early phases proves tougher. Hence, every healthcare provider should be vigilant about the potential occurrence of FGTB in patients exhibiting symptoms such as infertility, chronic pelvic pain, menstrual dysfunction, etc., and strive to recognize the disease in the early stages. Given that the medical and surgical treatment may fall short and also bearing in mind the irreversible organ damage FGTB can induce, patients can explore assisted reproduction as a valuable option to attain a successful pregnancy.
Fellowship in Reproductive Medicine course offered at Medline Academics offers a comprehensive curriculum which will equip the specialists with up-to-date knowledge and skills needed to manage patients with infertility and other co-existing complications. Make a meaningful influence in your patients’ life by enrolling in this course to expand your knowledge and skill sets, and also to be tuned to the recent developments in the field of assisted reproductive techniques.