Blastocyst transfer and culture
What are blastocysts?
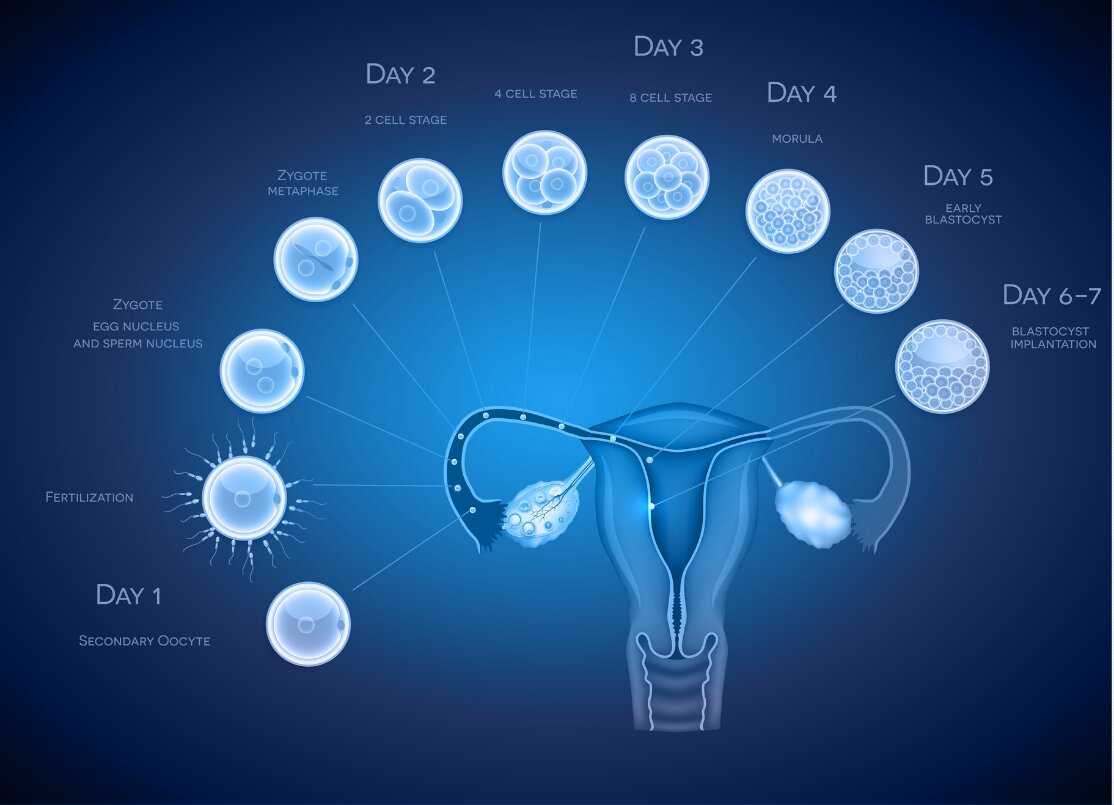
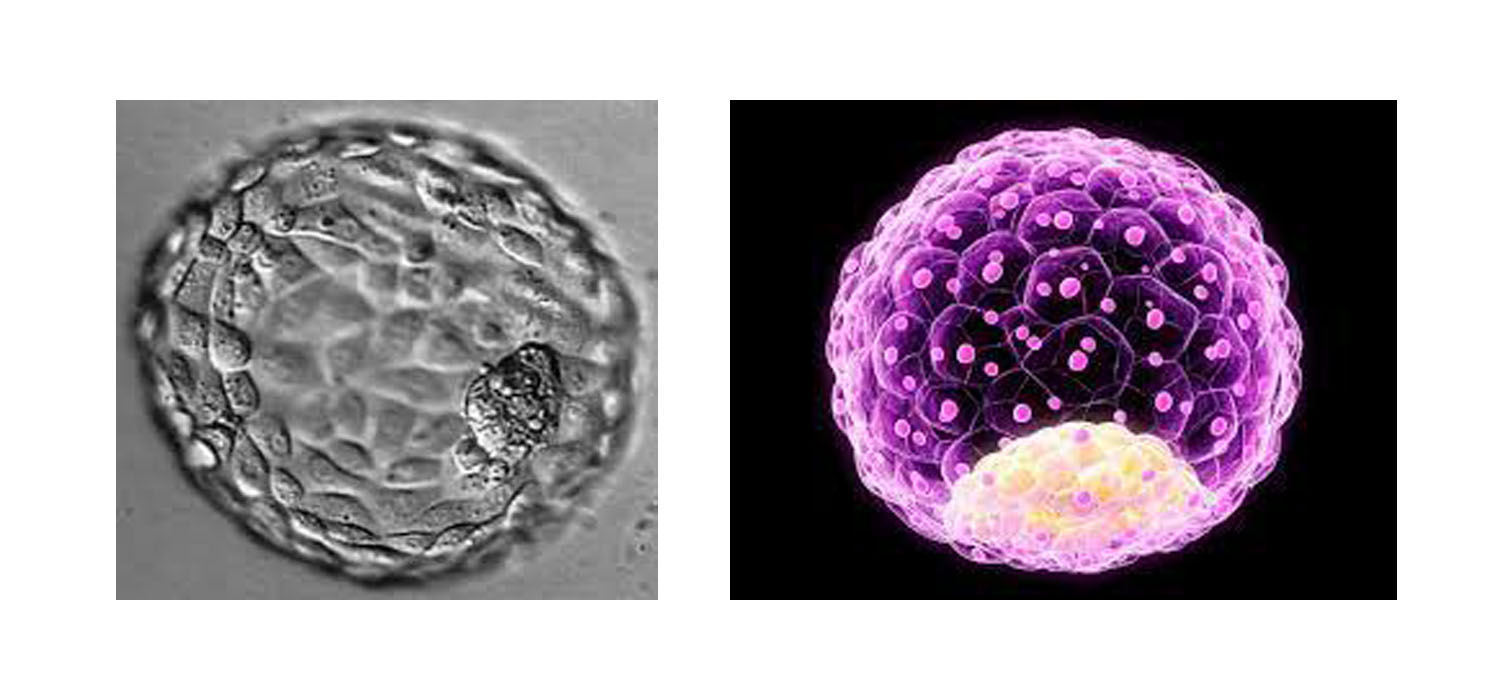
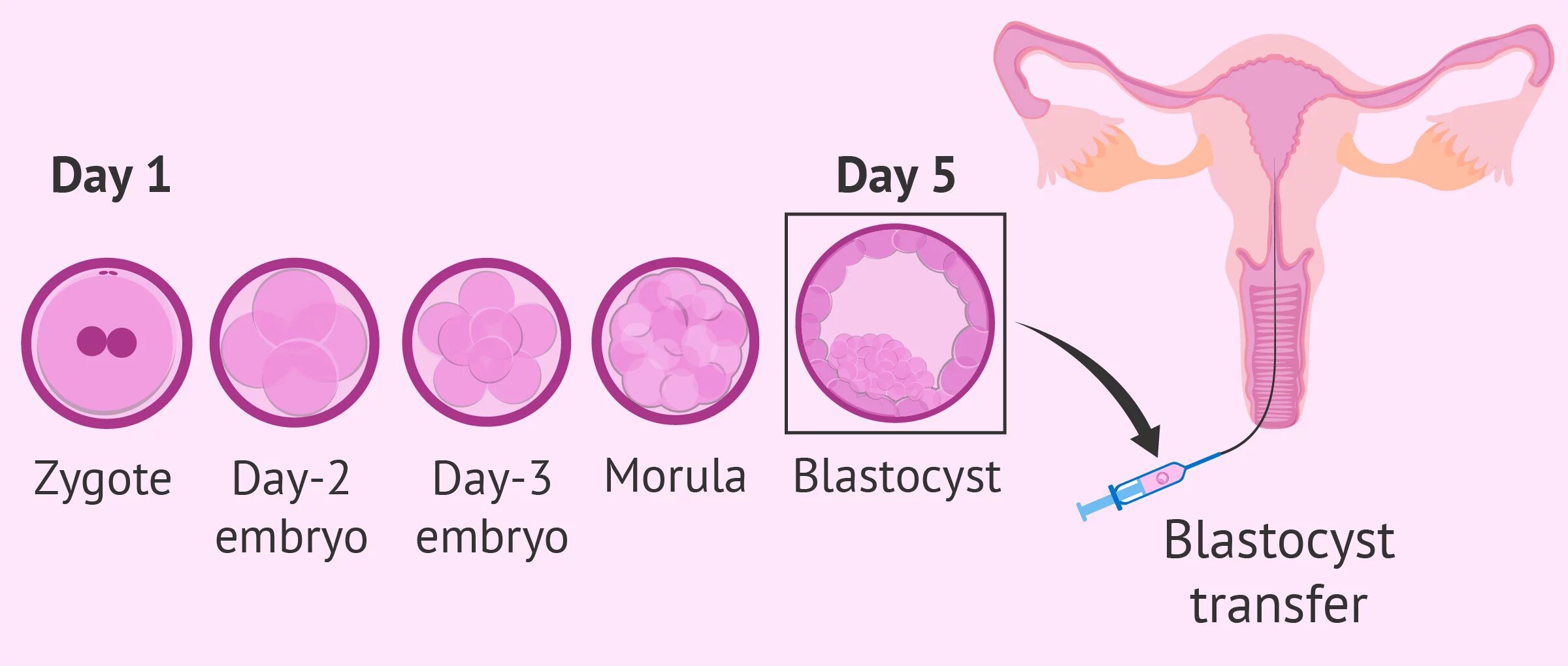
Fertilization of an egg by sperm results in the formation of a zygote or a fertilized egg. By three days, a healthy fertilized egg will have about 6 to 10 cells. By the fifth or sixth day, the fertilized egg is a fast-growing ball of cells, known as a blastocyst. Blastocyst contains about two different kinds of cell types and a central fluid-filled cavity. The first kind of cell is the inner cell mass (ICM) which will give rise to the foetus and the second layer of cells is called trophectoderm which gives rise to the placenta.
How is blastocyst cultured?
Previously invitro culture of embryos to the blastocysts stage using conventional media was unsuccessful. With scientific advancements and the development of culture media, it is now possible to culture fertilized eggs up to the blastocyst stage in a laboratory. However, it requires trained embryologists, quality control and optimal laboratory conditions to perform a successful blastocyst culture.
Why are blastocysts used in IVF?
In natural conception, fertilization occurs in the fallopian tube, and the fertilized egg moves and reaches the uterus. While traveling down the tube towards the uterus they undergo changes from the two-cell stage to the blastocyst stage by the time they reach the uterine cavity. Thus, the blastocyst stage is the stage of development where the implantation occurs in the uterus on day 5/6 when receptivity for implantation is particularly high. However, following conventional invitro fertilization, embryos are only at the four to eight-cell stage when they are transferred to the uterus. Hence transfer of blastocyst would be closer to the in vivo situation.
Secondly, in an IVF lab, oocytes retrieved from women are fertilized and grown until cleavage stage embryos. However not all these embryos may develop into blastocyst, only 60 to 70% of human embryos develop into the blastocyst stage after 5 days of culture. The remaining embryos perish even though they were healthy looking. This self-selection process enables only the best embryo to develop into the blastocyst stage. The embryos that survived to this stage are more likely to be healthy, robust and most competent to survive inside the uterus when transferred.
What is blastocyst transfer?
Generally, embryos formed by IVF or ICSI has been transferred into the women’s uterus on Day 2 or Day 3 after egg collection. Nonetheless, advances in the IVF laboratory and culture media now enables us to culture embryos beyond day 2 or day3 until the blastocyst stage. Since only the survival of the fittest reach the blastocyst stage by natural selection, embryologists were able to identify and transfer only the best embryos on Day 5 which has the crossed the phase of developmental arrest. They were also able to avoid healthy looking but naturally perishable embryos.
How are blastocysts classified?
The most standardized international classification system and worldwide used form of classification is Gardner and Schoolcraft classification. Blastocysts are classified based on the size and expansion, ICM (inner cell mass), and Trophectoderm as follows.
| Table 1. Gardner and Schoolcraft Classification System (Gardner et al., 2000; 2004) | |
|---|---|
| Size and expansion | |
| Classification | Description |
| 1 | Early blastocyst: the blastocele is less than half the volume of the embryo. |
| 2 | Blastocyst: the blastocele is greater than or equal to half of the volume of the embryo. |
| 3 | Full blastocyst: the blastocele completely fills the embryo. |
| 4 | Expanded blastocyst: the blastocele volume is larger than that of the early embryo and the zona pellucida is thinning. |
| 5 | Hatching blastocyst: the trophectoderm has started to herniate through the zona pellucida. |
| 6 | Hatched blastocyst: the blastocyst has completely escaped from the zona pellucida. |
| ICM (Inner Cell mass) | |
| Classification | Description |
| A | tightly packed, many cells |
| B | loosely grouped, several cells |
| C | very few cells |
| Trophectoderm (TE) | |
| Classification | Description |
| A | many cells forming a tightly knit epithelium |
| B | few cells |
| C | very few cells forming a loose epithelium |
Who will benefit from blastocyst transfer?
- Since only single best embryo with high quality is chosen and transferred during blastocyst transfer, it can be preferred for patients who would like to have only a single baby during pregnancy.
- Several studies have shown blastocyst transfer is useful for patients with previous multiple failed IVF with d2/d3 embryo transfer. It has been reported that the implantation and Pregnancy rate with blastocyst transfer is better in patients with at least 2 failed previous d2/d3 embryo transfer.
- For women who undergo repeated implantation failure, are of advanced maternal age or with family history of hereditary disorder would benefit from performing preimplantation genetic testing on the blastocysts. Preimplantation genetic testing or embryo biopsy analyses the complete chromosomal status of the embryo before embryo transfer. PGT will enable the doctors to avoid chromosomally abnormal embryos.
What are the Advantages of blastocyst transfer?
- As previously mentioned, self- selection process of the best embryos to become blastocysts allows us to choose only the healthy and best blastocyst for transfer.
- Several studies have shown that embryo transfer at the blastocysts stage results in higher implantation rates compared to cleavage stage day 2 or day 3embryo transfer.
- Blastocyst transfer has lower risk of multiple pregnancy.
- It also allows for performing Preimplantation genetic testing without risk to the developing fetus.
- Derivation of human embryonic stem (hES) cell lines from the ICM of the blastocyst.
- Recent advances
Non-invasive methods of PGT(niPGT) can analyse the genomic DNA from embryo culture medium or blastocyst cavity fluid providing a less invasive alternative to embryo biopsy.
What are the disadvantages of blastocyst transfer?
- One of the major disadvantages of blastocyst culture is that poor rates of blastocyst development in vitro and cancellation of transfer.
- Not all cleavage-stage embryos develop into blastocysts. Even if patients had many cleavage stage embryos they may not have any blastocysts available.
- Successful blastocyst culture requires optimal standardization and quality-controlled culture conditions.
- Monozygotic twinning incidence is more in blastocyst transfer then embryo transfer or natural pregnancy.
Embryologist training is vital in appropriately grading the blastocysts and transferring only the embryo with the greatest capability to proceed to gestation.
If you are interested to learn more about blastocyst culture and transfer, join Fellowship in embryology course by Medline academics.